Change Healthcare today announced Claims Lifecycle Artificial Intelligence, a new capability being integrated into the company’s Intelligent Healthcare Network and financial solutions, to help providers and payers optimize the entire claims processing lifecycle.Claims Lifecycle AI OverviewThis Change Healthcare Claims Lifecycle AI service is trained on more than 500 million service lines making up over 205 million unique claims that touch $268 billion in charges. The service leverages the
Read More
Healthcare Claims
Waystar Acquires UPMC’s Ovation Transaction Services Business for Enhanced Claims Monitoring Capabilities
Waystar(formerly known as ZirMed), a provider of healthcare revenue cycle management services, today announced it will be acquiring a major part of the transaction services technology business of Ovation, a health information management and management cycle solution currently owned and operated by University of Pittsburgh Medical Center (UPMC). Financial details of the acquisition were not disclosed.Ovation Transactions uses advanced algorithms to monitor claims at many health systems and
Read More
Change Healthcare Launches Front-End Denials Management Tool for Providers
Change Healthcare today unveiled a new technology that helps providers reduce one of the leading causes of claim denials. Assurance Attach Assist™, a module of Change Healthcare Assurance Reimbursement Management™, now anticipates what documentation a payer—including Medi-Cal and seven other payers—may require to help prevent the denial of a claim due to lack of documentation. The result: Providers can now use Assurance Attach Assist’s automation as a tool to proactively decrease
Read More
7 Reasons Why Claims Data Cannot Drive Patient Health Improvements
With the Department of Health and Human Services' decision to tie 90 percent of Medicare payments to value based models by this year, we can expect organizations to move even faster toward streamlining their population health management programs. But a survey from Managed Healthcare Executive notes that only 12% of survey respondents say their organization is using data “very well” and it’s making a “big impact” at their organization, the same percentage as 2016. Obviously there is still a steep
Read More
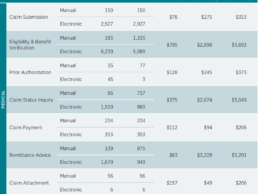
CAQH Index: Healthcare Claims Automation Could Save Industry $11B Annually
The U.S. healthcare industry made a modest amount of progress in healthcare claims automation, but a significant opportunity to save $11.1 billion annually remains, according to new data released today in the fifth annual CAQH Index. The report shows increased use of some manual transactions – primarily via web portals – resulting in a reversal of gains made for some of those transactions in previous years and the increase in potential savings. The $11.1 billion industry savings opportunity is
Read More
5 Key Components of A Results-Driven AI Platform for Hospitals and Health Systems in the Era of Value-based Care
Value-based reimbursement is forcing hospitals and health systems to reduce costs and to improve outcomes. Whether they are trying to manage population health or to improve clinical pathways in hospitals, healthcare organizations need a way to understand and harness the huge amounts of data that could potentially be applied to achieving these goals. Artificial intelligence (AI) systems offer an approach that can derive actionable insights from large, complex datasets at the scale required by
Read More
Reimbursify Launches New App for Out-of-Network Reimbursement Claims
Reimbursify, a healthcare-focused technology company providing app-centric solutions for consumers, healthcare providers & businesses has launched a new app that gives patients a quick and easy way to file out-of-network reimbursement claims with their insurance company in less than 60 seconds. Users can also monitor their current, pending, and past claims from the app. Reimbursify is currently being used by patients in 21 states as well as Puerto Rico."Visits to healthcare providers who
Read More
3 Key Areas An Automated Prior Authorization Solution Must Address
Editor's Note: Co-written by Scott Herbst, Senior Vice President and General Manager of Provider Solutions and Ryan Miller, Senior Vice President of Strategy & Corporate Development at Availity.Prior authorizations may be as popular among providers as ants at a picnic, but they have become a common and necessary part of the reimbursement process. As a result, being able to manage prior authorizations efficiently is critical to maintaining a healthy revenue cycle and avoiding issues such as
Read More
Change Healthcare: $262B in Healthcare Claims Initially Denied in 2016
A new analysis by Change Healthcare of $3 trillion in medical claims submitted to payers last year revealed 9% of charges, representing $262 billion, were initially denied. For the typical health system, as much as 3.3% of net patient revenue, an average of $4.9 million per hospital, was put at risk due to denials. While 63% of these claims were recoverable on average, reworking each denial costs providers roughly $118 each, or as much as $8.6 billion in appeals-related administrative
Read More
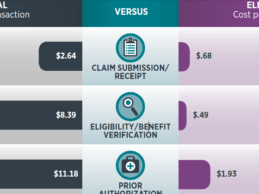
Report: Reducing Manual Business Transactions Could Save Healthcare $9.4B
Reducing manual business transactions could save healthcare $9.4 billion in savings, according to new data released today in the fourth annual 2016 CAQH Index. The index reveals that conducting resource-intensive manual transactions are costing U.S. health plans and healthcare providers as much as $11 more per transaction and on average $6 more than when conducted electronically. CAQH Index Overview The fourth annual CAQH Index measures adoption, costs and, for the first time, provider labor
Read More