- Allscripts has certified Redox as the first global integration engine of the Allscripts Developer Program (ADP).- Redox provides a single, global connection to Allscripts Unity APIs that digital health vendors can use to integrate and exchange data with approved Allscripts client sites.- All digital health vendors that are part of the Redox Interoperability Network will automatically be eligible for Allscripts Unity API access; these digital health vendors benefit from faster implementation
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
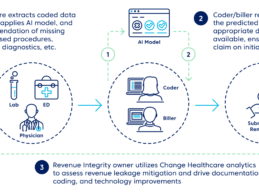
Change Healthcare Unveils AI-Infused Charge Capture for Providers
- Change Healthcare unveils a new AI solution, Charge Capture Advisor that will help providers capture more revenue—automatically.
- Charge Capture Advisor identifies potentially missing charges for services that providers performed before claims are submitted.
- Change Healthcare’s AI for charge capture is trained on more than 500 million service lines and 180 million unique, de-identified claims that touch $245 billion in charges.
Change Healthcare today introduced Charge
Read More
Baptist Health South Florida Launches Spanish and English Patient Access Solutions
Quick Glance- Baptist Health South Florida launches new online patient access experience for consumers with technology from Kyruus- Solution enhances digital capabilities for Both English- and Spanish-Speaking consumers in the greater Miami areaKyruus announced that Baptist Health South Florida is now leveraging its ProviderMatch for Consumers and ProviderMatch® for Consumers in Spanish solutions. As a result, English- and Spanish-speaking patients in the Greater Miami Area can easily search for
Read More
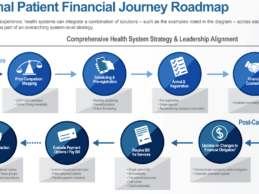
Dysfunctional Patient Billing Major Distraction for Patients & Clinicians
Dysfunctional patient billing is a major distraction for both patients and clinicians, according to recent research conducted by HIMSS in partnership with OODA Health. The research report reveals patients are distracted by bills and payment concerns resulting in a lower level of compliance and adherence to medical plans. Clinicians are distracted by clerical/financial tasks that limit time with or take time away from patients. This research complicates the simple construct of patient billing as
Read More
How Will FY2020 IPPS Proposed Rule Affect Hospital CDI Programs?
In April, Centers for Medicare and Medicaid Services (CMS) released the fiscal year (FY) 2020 inpatient prospective payment systems (IPPS) proposed rule. The proposed rule notably includes approximately 1,500 complications or comorbidities (CC)/major complications or comorbidities (MCC) designation changes and 324 changes to International Classification of Diseases (ICD)-10-CM codes, along with several other updates. The designation changes are an effort to respond to the notion that the
Read More
10 Considerations for Success In A Post-MACRA Value-Based Healthcare Reality
The first two years of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) Quality Payment Program (QPP) are in the books and many organizations are wondering if their strong performances will ever be met with a significant upside adjustment.
Year 1 (2017) enjoyed very high participation levels, 95% of eligible clinicians, but very low upside adjustments. Between the Test Pace option, artificially low bar (3 points) for an upside adjustment, and numerous opportunities to score
Read More
Report: Health Systems Are Struggling to Simplify Patient Billing & RCM Processes
Today’s health systems are prioritizing patient financial experiences, yet many still struggle to simplify patient billing and align it with revenue cycle management (RCM), according to an in-depth study, commissioned by patient payment and engagement platform Cedar and conducted by The Health Management Academy (The Academy). The Cedar and Academy study examined practices at 20 of the top 100 U.S. health systems including qualitative and quantitative analyses of 23 senior executives
Read More
Norton Healthcare Goes Live on Kyruus ProviderMatch Patient Access Platform
Norton Healthcare, a not-for-profit health system based in Louisville, has deployed the Kyruus patient-provider matching solutions to enhance patient access across its five hospitals, 14 urgent care clinics, and 190 medical practices. Now working with Kyruus, Norton Healthcare is empowering consumers to choose the providers that best suit their unique clinical needs and personal preferences for both adult and pediatric care.Enterprise-Wide Provider DirectoryBefore deploying ProviderMatch for
Read More
M&A: Experian Acquires Care Coordination Platform MyHealthDirect
Experian has acquired MyHealthDirect, a developer of digital care coordination solutions based in Nashville that optimizes scheduling and care planning for providers, payers and consumers. The move gives Experian’s health business a strategic boost as it continues enabling clients to meet the changing demands of consumers – in particular, demands around removing complexity and increasing transparency in healthcare. Financial details of the acquisition were not disclosed. Growing Importance of
Read More
Research: Half of Hospital Leaders Plan to Invest in AI by 2021
Half of hospital leaders plan to invest in artificial intelligence (AI) and robotic process automation (RPA) solutions by 2021, according to a new study conducted by Olive AI that reveals AI adoption healthcare is still in its infancy. The study explores how hospital leaders are responding to the imperative to drive efficiency and reduce costs through strategic investments in non-clinical technologies. Conducted in partnership with Sage Growth Partners, the survey respondents included 115
Read More