Today’s health systems are prioritizing patient financial experiences, yet many still struggle to simplify patient billing and align it with revenue cycle management (RCM), according to an in-depth study, commissioned by patient payment and engagement platform Cedar and conducted by The Health Management Academy (The Academy). The Cedar and Academy study examined practices at 20 of the top 100 U.S. health systems including qualitative and quantitative analyses of 23 senior executives collectively managing more than $89 billion in operating revenue.
Patient Billing Driven by Antiquated Processes & Impersonal Experiences
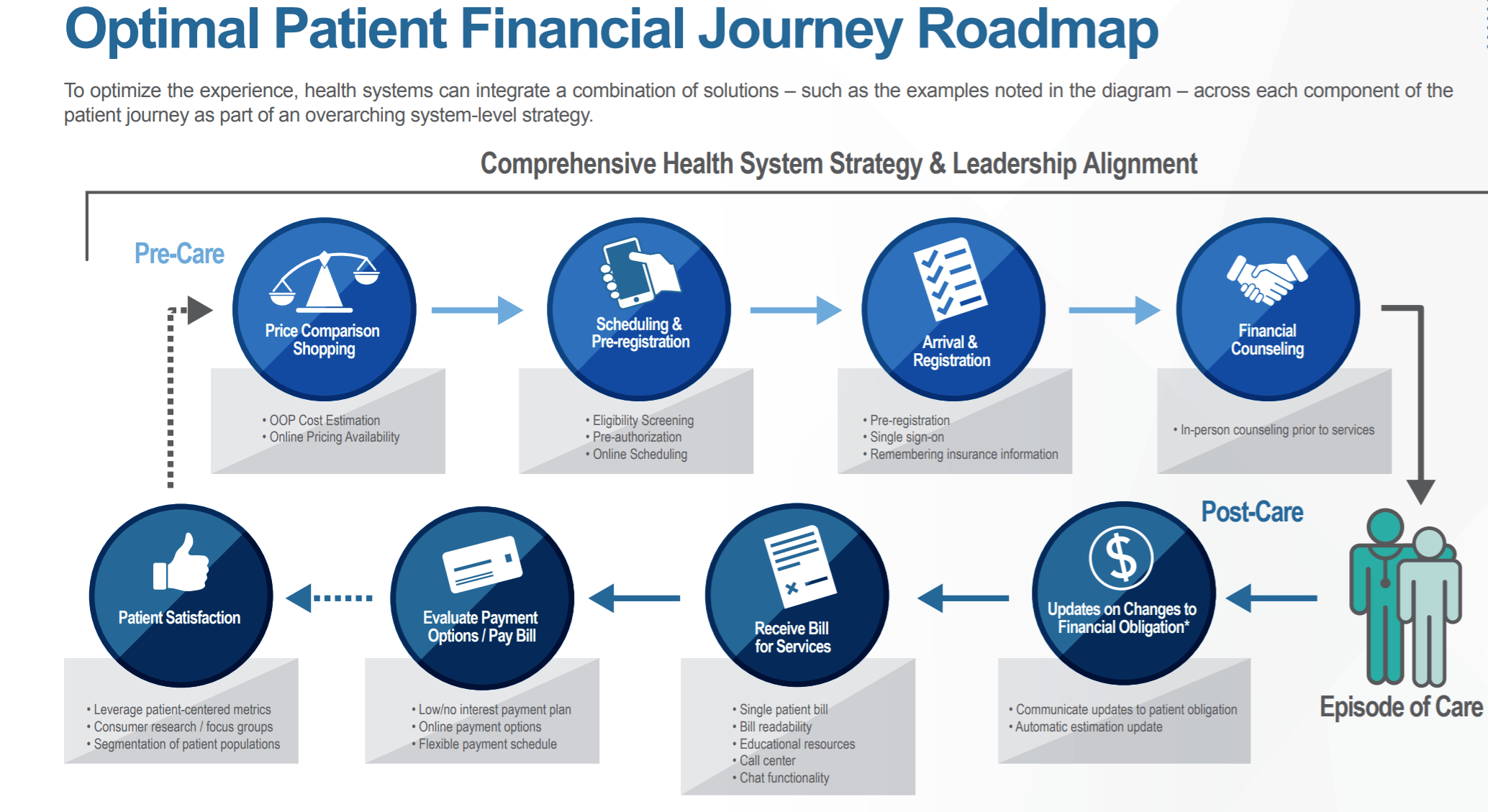
Patient billing is often driven by antiquated processes and impersonal experiences, which can lead to consumer confusion. As a result, regulatory pressure has mounted to improve price transparency. The study found that more than half of executives identify consumer-centric financial experiences among their top priorities. In addition, 63% are aligning at least four of the eight points across the pre-, during- and post-care patient financial journey (e.g. scheduling, account creation, billing, final payment).
Barriers to Improve Patient Billing
The study also revealed that health system executives mainly think in terms of internal operational challenges as opposed to external issues (policy, regulations or consumer expectations) as the biggest barriers to improving patient billing experiences. Finance executives believe that competing priorities are the most common barrier to improving patient billing (75%), while Consumer executives believe that patient engagement is the most common barrier (80%).
Consumer-Friendly Methods Are Imperative to Optimizing Patient Financial Experience
While the industry has made solid strides, some health systems still need to integrate more consumer-friendly methods of engagement like consolidated bills, more flexible payment plans and pre-care price transparency tools.
Specifically, the study data indicated that health systems should continue:
1. Increasing flexibility in patient payment plans
A strong 82% of top health systems offer flexibility with low- or no-interest payment plans to consumers based on factors like credit scores. However, only 41% offer self-select payment plans, which gives consumers more control over their financial responsibility.
2. Providing more consumer-friendly resources
A key priority for health systems is offering more accessible resources that help patients understand expected charges. Currently, 65% of health systems have out-of-pocket price estimators for patients before they receive care. That said, a greater amount (80%) are posting chargemasters, which can make obtaining accurate, real-time cost estimations a challenge, as they often don’t reflect actual patient responsibility.
3. Consolidating bills
While many health systems are leveraging alternative billing methods (e.g. patient portal, online billing applications), 35% don’t offer a consolidated bill. Of those that do, it usually only includes charges from within the health system (hospitals, providers, post-acute care, home care, etc.). As patients often see many affiliated service providers in one episode of care, most will still receive multiple bills in different formats, at different times, and with different payment terms – adding to patient confusion.
4. Driving adoption of tracking patient-centric metrics
An increasing amount of top health systems are incorporating patient-centric metrics tracking in their RCM strategy, but that is still well behind the tracking of more traditional RCM metrics that focus on their own financial well-being. All health systems track net collection ratios and claims denial rates, but only some are including patient-centric metrics like patient satisfaction (67%), time to bill (58%), self-serve (33%), and bill readability (25%).
5. Implementing end-to-end RCM technology
Only 41% of top health systems use an end-to-end RCM solution, with 50% using RCM tech for one or more RCM components and 8% not using one at all.
6. Bridging disconnect between finance and consumer executives
The study found 80% of health system consumer executives reported patient engagement as a significant barrier to improving patient billing, while 75% of finance executives rated competing priorities as the top barrier.
Why It Matters
“It’s great to see that the top health systems are prioritizing the patient financial experience, but there is still much room for improvement. Approximately three in 10 Americans have experienced a healthcare bill go to collections, and if the top health systems are still facing challenges, then that indicates that the whole ecosystem has more work to do,” said Florian Otto, co-founder and CEO of Cedar. “Overall, the U.S. healthcare system still doesn’t offer the same seamless experience that consumers have come to expect in other industries such as retail or banking. This study demonstrates that the recognition is present, but many challenges remain.”
Report Background/Methodology
In May and June of 2019, The Health Management Academy conducted a series of quantitative and qualitative assessments with senior Leading Health System executives regarding the patient financial experience. The 23 total respondents represent 20 unique health systems. Respondent roles included Chief Financial Officers, VP of Revenue and Treasury, System Director – Patient Financial Services, VP of Revenue Cycle, VP of Patient Financial Services, Chief of Staff, Chief Officer of Strategic Communication, and Senior Vice President.
