- CVS Specialty launches Specialty Expedite, a pharmacy solution that uses technology to significantly streamline the process and keep patients informed of the status of their prescription along the way.
- Streamlined prior authorization and benefits verification process using connectivity with EHR platforms, helping patients get their medications in as little as three days.
- Patients are also able to choose how they want to get their specialty medications – at their local CVS
Read More
Prior Authorization
DrFirst Integrates Adobe Sign With Backline Secure Care Collaboration Platform
- DrFirst and Adobe Sign has announced the integration of Adobe Sign e-signature solution with DrFirst’s Backline secure care collaboration platform, producing the first mobile solution for the healthcare market to offer an e-signature capability.
- Using the joint solution, providers can send SMS messages to the mobile devices of patients, caregivers, or other clinicians to share documents that require signatures.
- Once received, the patient or provider can tap a link in the text
Read More
DrFirst Integrates with Epic’s Real Time Prescription Benefits Prescribing Workflow
DrFirst, a provider of e-prescribing, price transparency, and medication management solutions announced today that it has entered into an integration agreement with leading EHR provider Epic to make DrFirst’s myBenefitCheck (real-time benefit check) service available to clients in Epic’s RTPB (Real-Time Prescription Benefits) prescribing workflow to help doctors and patients understand the cost of the drugs and drive medication adherence.How myBenefitCheck WorksVia myBenefitCheck, prescribers
Read More
Waystar Acquires AI Firm Digitize.AI to Tackle Prior Authorizations
Bain-Capital-backed revenue cycle management company Waystar is acquiring Digitize.AI, an artificial intelligence firm, to enable faster and smarter prior authorizations in healthcare – one of the largest pain points for both providers and consumers.Financial Impact of Prior AuthorizationsPrior authorizations, the process by which insurance companies and payers determine if they will cover a prescribed procedure or medication, are meant to help patients avoid surprise bills and unexpected
Read More
Olive, Clinc Partner to Add Conversational AI to Digital Healthcare Employee for Hospitals
Olive, the company that introduced healthcare’s AI-driven digital employee has joined forces with Clinc, another trailblazer in Artificial Intelligence (AI), to free up time and resources by adding conversational AI capabilities to its existing technology. The combined offering allows Olive’s digital healthcare employee to bring hospitals and health systems broader applications across revenue cycle, supply chain and other financial and operational departments.
While new technologies
Read More
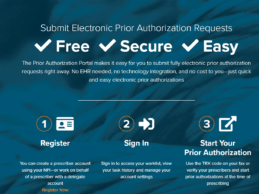
Surescripts Inks Partnerships with National Health Plans to Streamline Prior Authorization
Surescripts announced that several national, regional and local PBMs and health plans representing virtually all U.S. patients are replacing their manual prior authorization process with Surescripts Electronic Prior Authorization solution. Over the past 18 months, several national, regional and local PBMs and health plans representing virtually all U.S. patients have signed on, increasing the number of insured lives covered by Surescripts Electronic Prior Authorization by nearly 20%.Impact of
Read More
Allscripts Acquires Prescription & Prior Authorization Platform ZappRx
EHR vendor Allscripts has reached an agreement to acquire prescription and prior authorization platform ZappRx, according to CNBC. The acquisition will help Allscripts diversify its business outside of electronic medical record (EHR). The company has raised a total of $40M in funding to date.Founded in 2012 by Zoe Barry who previously worked at athenahealth, ZappRx streamlines the complex process required to order specialty medications, increasing efficiencies when collecting and maintaining the
Read More
Humana Integrates Real-Time Benefits Tool with Epic’s E-prescribing Workflow
Humana and Epic today announced an agreement to integrate Humana’s IntelligentRX real-time benefits tool directly into Epic’s e-prescribing workflow. Humana is the first national insurer to collaborate with Epic to bring together patients, providers and payers to power value-based care. The resulting integration will deliver real-time pharmacy data and access to patient’s medical history, which, in turn, will enable cost reduction, improved quality, and increased patient
Read More
DrChrono Integrates with CoverMyMeds to Expedite Prior Authorization Processing
DrChrono, today announced its expanded partnership with CoverMyMeds to help providers expedite prior authorization processing, gain insight into prescription prices and help patients get the medication they need when they need it.DrChrono/CoverMyMeds Integration DetailsDrChrono’s integration with CoverMyMeds includes:· RxBenefit Clarity - RxBenefit Clarity is a medication decision support platform that displays the most accurate prescription price information at the point of prescribing. This
Read More
XIFIN Expands Patient and Physician Engagement Capabilities
XIFIN announced the expansion of its portfolio of physician and patient engagement solutions with integrated patient responsibility estimation and automated prior authorization capabilities, enabling diagnostic providers to improve their patient experience and physician satisfaction. The new capabilities include a strategic partnership with Glidian that integrates automated prior authorization capabilities with XIFIN’s revenue cycle management and laboratory information system solutions, XIFIN
Read More