Surescripts announced that several national, regional and local PBMs and health plans representing virtually all U.S. patients are replacing their manual prior authorization process with Surescripts Electronic Prior Authorization solution. Over the past 18 months, several national, regional and local PBMs and health plans representing virtually all U.S. patients have signed on, increasing the number of insured lives covered by Surescripts Electronic Prior Authorization by nearly 20%.Impact of
Read More
Prior Authorization
Allscripts Acquires Prescription & Prior Authorization Platform ZappRx
EHR vendor Allscripts has reached an agreement to acquire prescription and prior authorization platform ZappRx, according to CNBC. The acquisition will help Allscripts diversify its business outside of electronic medical record (EHR). The company has raised a total of $40M in funding to date.Founded in 2012 by Zoe Barry who previously worked at athenahealth, ZappRx streamlines the complex process required to order specialty medications, increasing efficiencies when collecting and maintaining the
Read More
Humana Integrates Real-Time Benefits Tool with Epic’s E-prescribing Workflow
Humana and Epic today announced an agreement to integrate Humana’s IntelligentRX real-time benefits tool directly into Epic’s e-prescribing workflow. Humana is the first national insurer to collaborate with Epic to bring together patients, providers and payers to power value-based care. The resulting integration will deliver real-time pharmacy data and access to patient’s medical history, which, in turn, will enable cost reduction, improved quality, and increased patient
Read More
DrChrono Integrates with CoverMyMeds to Expedite Prior Authorization Processing
DrChrono, today announced its expanded partnership with CoverMyMeds to help providers expedite prior authorization processing, gain insight into prescription prices and help patients get the medication they need when they need it.DrChrono/CoverMyMeds Integration DetailsDrChrono’s integration with CoverMyMeds includes:· RxBenefit Clarity - RxBenefit Clarity is a medication decision support platform that displays the most accurate prescription price information at the point of prescribing. This
Read More
XIFIN Expands Patient and Physician Engagement Capabilities
XIFIN announced the expansion of its portfolio of physician and patient engagement solutions with integrated patient responsibility estimation and automated prior authorization capabilities, enabling diagnostic providers to improve their patient experience and physician satisfaction. The new capabilities include a strategic partnership with Glidian that integrates automated prior authorization capabilities with XIFIN’s revenue cycle management and laboratory information system solutions, XIFIN
Read More
Inova Personalized Health Accelerator Invests in Prior Authorization Platform, CoverMyTest
Inova Personalized Health Accelerator (IPHA), an unique program providing health IT entrepreneurs with C-suite coaches, early-stage capital and strategic partners, today announced it has invested in health IT startup CoverMyTest. The New York-based startup partners with labs to optimize and automate prior authorization (PAs) workflows.CoverMyTest is the only PA service provider solely focused on assisting laboratories offering genetic and genomic testing. This PA software comes at a critical
Read More
3 Key Areas An Automated Prior Authorization Solution Must Address
Editor's Note: Co-written by Scott Herbst, Senior Vice President and General Manager of Provider Solutions and Ryan Miller, Senior Vice President of Strategy & Corporate Development at Availity.Prior authorizations may be as popular among providers as ants at a picnic, but they have become a common and necessary part of the reimbursement process. As a result, being able to manage prior authorizations efficiently is critical to maintaining a healthy revenue cycle and avoiding issues such as
Read More
Chilmark: New Prior Authorization Solutions Can Address Provider-Payer Friction
Prior Authorization is often viewed as the poster child for throwing the Quadruple Aim off balance with its pursuit of cost reduction at the expense of provider experience, but the latest research from Chilmark Research shows that new PA models and maturing PA technology solutions could benefit both providers and payers.Traditionally, primitive PA and its associated impacts account for the great divide in provider-payer relationships. The sheer volume of PA requirements is getting increasingly
Read More
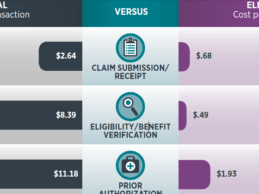
Report: Reducing Manual Business Transactions Could Save Healthcare $9.4B
Reducing manual business transactions could save healthcare $9.4 billion in savings, according to new data released today in the fourth annual 2016 CAQH Index. The index reveals that conducting resource-intensive manual transactions are costing U.S. health plans and healthcare providers as much as $11 more per transaction and on average $6 more than when conducted electronically. CAQH Index Overview The fourth annual CAQH Index measures adoption, costs and, for the first time, provider labor
Read More
Cerner, CoverMyMeds Integrate to Accelerate Electronic Prior Authorization Process
Cerner and CoverMyMeds are announcing this morning an agreement to integrate CoverMyMeds’ ePA within Cerner’s Millennium EHR. The advanced functionality will provide more than 350,000 e-prescribing end-users the ability to accelerate the prescription review process by removing manual processes and helping to reduce transaction costs. CoverMyMeds will provide Cerner physicians the capability to process requests electronically in seconds and receive notification of a patient’s authorization status
Read More