The new administration shed light on policy issues at the top of providers’ lists for 2025. While topics like physician burnout and Medicare payment reform were included, unsurprisingly, prior authorization remains at the forefront, as proven by entities like the American Medical Association, who represent more than 270K providers. Improvements in the prior authorization and interoperability space have been historically stalled due to lack of standard data and public reports, as technology
Read More
Prior Authorization
Humata Health’s AI-Powered Prior Authorization Platform Now Available on Microsoft Azure Marketplace
What You Should Know:
- Humata Health, a provider of AI-powered touchless prior authorizations, today announced the availability of its platform in the Microsoft Azure Marketplace, an online store providing applications and services for use on Azure.
- The integration allows healthcare payers and providers seeking to automate prior authorization to leverage the productive and trusted Azure cloud platform, with streamlined deployment and management.
Transforming End-to-End
Read More
85% of Cancer Patients Face Unnecessary Insurance “Red Tape” Due to Prior Authorization, Says New CancerCare Report
What You Should Know:
- A new national survey from CancerCare reveals how insurance utilization management practices, particularly prior authorization, create serious and stressful barriers to care for cancer patients. The report, titled "The Health Insurance Maze: How Cancer Patients Get Lost in the Red Tape of Utilization Management," found that these requirements frequently delay diagnosis and treatment, adding significant "time toxicity" to patients' lives.
- The
Read More
RISA Labs Raises $3.5M for AI-Powered Oncology Prior Authorizations Platform
What You Should Know:
- Cancer patients don’t just fight the disease - they fight the system. Today, life-saving treatments are routinely delayed by days or even weeks due to manual, error-prone workflows
- To solve this, RISA Labs has raised a $3.5M funding round to help healthcare organizations eliminate one of the most persistent barriers to timely cancer care: prior authorization delays. RISA Labs has already proven that faster care is possible by dramatically reducing manual
Read More
WEDI Survey: Industry Readiness for CMS Interoperability and Prior Authorization Rule
What You Should Know:
- The Workgroup for Electronic Data Interchange (WEDI) has published the results of its baseline survey, assessing the healthcare industry's preparedness to meet the requirements of the Centers for Medicare & Medicaid Services (CMS) Advancing Interoperability and Improving Prior Authorization Final Rule (CMS-0057-F).
- This rule introduces new provisions aimed at increasing data sharing, including Patient Access, Provider Access, Payer-to-Payer,
Read More
AI-Driven Prior Authorization Denials Raise Concerns Among Physicians, AMA Survey Reveals
What You Should Know:
- A new survey from the American Medical Association (AMA) reveals growing concern among physicians about the use of artificial intelligence (AI) in prior authorization decisions by health insurers.
- The survey found that 61% of physicians are worried that AI-powered tools are leading to an increase in prior authorization denials, potentially harming patients and contributing to unnecessary healthcare costs.
Prior Authorization Concerns
Prior
Read More
Revitalizing Medicare Advantage: How The Push to Streamline Prior Authorization Will Impact Senior Care
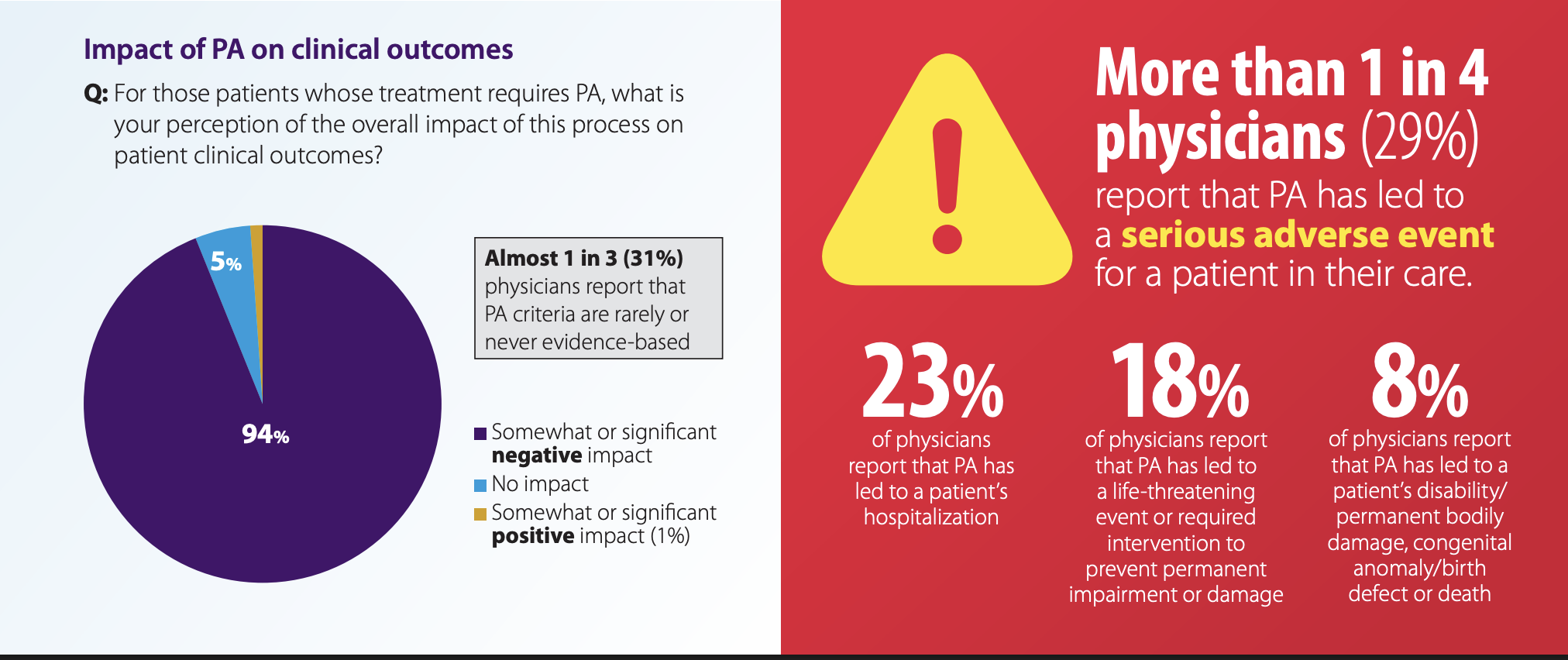
As a physician, the odds that you’ve had a negative experience related to the prior authorization process are (unfortunately) highly likely. According to the American Medical Association’s (AMA) 2023 Prior Authorization Physician Survey, 1 in 4 physicians report that prior auths “have led to a serious adverse event for a patient in their care.” Think about the toll that this takes on professionals whose primary job is providing lifesaving care, and the thing preventing this care is outside their
Read More
Q/A: Vim CEO Talks Solving the Rising Tide of Healthcare Claim Denials
The U.S. healthcare system is grappling with a surge in claim denials and prior authorization requirements, creating significant challenges for both providers and patients. To shed light on this pressing issue, we spoke with Oron Afek, CEO of Vim, a company that assists over 20,000 providers and 80% of the largest U.S. payers with prior authorizations.
In this interview, Oron Afek provides valuable insights into the challenges and potential solutions related to claim denials and prior
Read More
HLTH: Blue Shield of California, Salesforce Partner on Real-Time AI Prior Authorizations
What You Should Know:
- Blue Shield of California and Salesforce are joining forces to tackle a major pain point in healthcare: the lengthy and often frustrating process of prior authorizations.
- The new AI-powered platform solution, built on Salesforce Health Cloud, aims to deliver near real-time prior authorization decisions, streamlining healthcare delivery and improving patient experience.
Addressing the Burden of Prior Authorizations
Prior authorizations are a
Read More
Transforming Insurance Verification and Authorizations with AI
Across many healthcare organizations, front-office staff face a significant dilemma: patients seeking help only to be told that their health insurance verification and authorization process could take several days or even months. According to a study by the AMA, more than nine in ten physicians recently surveyed said that prior authorization negatively impacts patient clinical outcomes and, often, leads to treatment abandonment.
This issue mainly arises because current, manual insurance
Read More