EHR leader Cerner, today announced that Zane Burke will step down as President of the company, effective Nov. 2. Effective immediately, John Peterzalek, Executive Vice President of Worldwide Client Relationships, will assume Burke’s responsibilities and the title of Chief Client Officer.“We thank Zane for his contributions to Cerner across more than two decades,” said Cerner Chairman and CEO Brent Shafer. “Zane leaves the company with a strong client focus and commitment to continued innovation,
Read More
Health IT | News, Analysis, Insights - HIT Consultant
Ciox Addresses CMS Fax Elimination Challenge: Believes Mandate is Necessary to Achieve a Fax-free Future
Since 2014, the healthcare industry has invested more than $17 billion[1] in digital integration and analytic capabilities to support care delivery, wellness and research. Despite new innovations, the use of fax machines remains a brittle link in the coordination and delivery of healthcare. Ciox, a healthcare technology company, sees a future without faxing and supports efforts by the Office of the National Coordinator for Health Information Technology and Centers for Medicare and Medicaid
Read More
DCH Health System to Implement MEDITECH Expanse EHR Across Enterprise
DCH Health System, a Tuscaloosa, AL-based health system has announced the decision to implement the MEDITECH Expanse EHR across select hospitals and clinics. The intuitive, web-based, mobile EHR system will equip DCH providers and clinicians with the enhanced tools necessary to increase their productivity.DCH Health System includes DCH Regional Medical Center, a 583-bed regional trauma and referral center; Northport Medical Center, a 204-bed community hospital with inpatient rehabilitation and
Read More
Blue Cross Blue Shield Association Taps Edifecs to Drive FHIR Adoption
Blue Cross Blue Shield Association (BCBSA), today announced that it has chosen Edifecs as a partner to help drive FHIR adoption across BCBS companies. FHIR is the future of interoperability, and FHIR standards can resolve many of the healthcare industry’s critical business issues. As part of the partnership, Edifecs’ user-friendly Edifecs XEngine Server Module for FHIR will be offered to BCBS companies to support the rapid deployment of these data standards with minimal training required. What
Read More
Livongo Health and Abbott Partner to Offer Continuous Glucose Monitoring Insights
Livongo Health, a consumer digital health company empowering people with chronic conditions to live better and healthier lives, today announced that it will be the first comprehensive offering for people with diabetes to integrate continuous glucose data from Abbott’s FreeStyle® Libre Pro System, a revolutionary continuous glucose monitoring (CGM) system for healthcare professionals.Through this integration collaboration, Livongo will offer, where appropriate and prescribed, the FreeStyle Libre
Read More
OnlyBoth Launches AI-Driven Hospital Benchmarking Engine
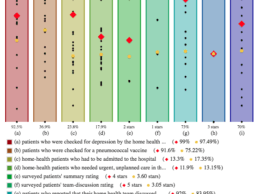
OnlyBoth Inc., a Pittsburg, PA-based healthcare performance company has launch an artificial intelligence (AI)-driven benchmarking engine BenchMine.com that provides objective, data-based comparisons of U.S. hospital performance. The Artificial Intelligence (AI)-based technology makes use of 130 consumer-friendly data attributes on 4,797 hospitals from CMS Hospital Compare to help the community evaluate hospitals and compare them to others nearby and nationally.Enhanced with geolocation
Read More
What The Patient Engagement Metrics Aren’t Telling You
The tech industry loves to tout high-level metrics to garner attention for apps: the success of an app is often demonstrated by quoting staggering numbers of subscribers, weekly views, in-app session length, number of downloads, monthly average users, etc. And these statistics are not irrelevant -- they are useful for gauging product performance and often correlate to a successful product. For apps driven by ad-revenue, they are sometimes the most important metrics.But as I address elsewhere,
Read More
Optimizing Revenue Cycle Management – What Will It Take to Get There?
The U.S. healthcare system is undergoing a major transformation, from many freestanding hospitals and individual practices to fewer large, integrated healthcare systems. One motivating factor is the promise of greater efficiencies when it comes to delivering more holistic patient care and improving core operational processes.Revenue cycle management is one process that’s primed for improvement. Poor billing practices can cost hospitals millions of dollars due to lost reimbursement or the
Read More
MEDITECH Integrates Prescription Drug Monitoring Programs (PDMP) Within Expanse EHR
EHR provider MEDITECH, today announced it is integrating one-tap access to state-regulated electronic Prescription Drug Monitoring Programs (PDMP) that track controlled substance prescriptions, from directly within the MEDITECH Expanse EHR.MEDITECH Expanse EHR Integration DetailsAvailable from DrFirst, the PDMP database link allows prescribers to view controlled substance histories effortlessly from multiple PDMPs simultaneously as allowed by cooperating states, within the EHR prior to
Read More
Innovaccer Launches EHR-Agnostic Physician Engagement Solution
The role of physicians is instrumental in the rapidly-transforming healthcare. There have been many strategic initiatives or restructured payment models- but the physicians have almost always been disconnected. Physicians are either overburdened with the data around them or have limited real-time visibility into the analyzed data.Limited access to the right data at the right time has dramatically increased the number of burned out physicians in the country. Additionally, the time-taking tasks of
Read More