As an industry, moving to electronic prescribing has changed the way clinicians, pharmacists and patients communicate about drug therapies. New data released today from Surescripts reports that e-prescription accuracy has increased by 64% since 2016. Thanks to this improvement, the handwritten doctor’s note that was often illegible or lost in transit is now a secure, digital transaction.Despite Growth, Challenges RemainsE-prescribing changed the way patients, prescribers and pharmacists
Read More
Pharmacy | Medication Adherence Technology Services and Solutions | News, Analysis, Insights - HIT Consultant
EMR Integration Is Key to Success for Drug Diversion Monitoring, KLAS Report Finds
EMR integration dramatically improves customer success with drug diversion monitoring solutions, according to a new KLAS Report. The new report reveals that EMR integration with drug diversion monitoring enables analytics tools to compare drug-use data from the eMAR, not just pharmacy systems. This integration closes the loop on the full medication administration process, improving accuracy, and creating a more complete picture for investigation.State of Drug Diversion Monitoring Solutions in
Read More
Only 20% of Customers Use A Pharmacy’s Mobile App, J.D. Power Finds
Only 20% of customers use a pharmacy’s mobile app, but those who did have satisfaction scores as much as 23 points higher than those who do not, according to the J.D. Power 2019 U.S. Pharmacy Study. The study reveals that despite the looming threat of disruption at the hands of e-commerce, the U.S. pharmacy industry continues to enjoy superior levels of customer satisfaction in both the brick-and-mortar and mail order segments.Other key findings of the 2019 study include:- Face-to-face
Read More
KLAS: Epic, Cerner, Lack Integration for Medication Inventory Management
Pharmacy and EMR vendors Cerner and Epic all have gaps in their ability to provide enterprise medication inventory management (MIM) capabilities, resulting in lower consideration rates in MIM purchase decisions, according to the latest KLAS report. The KLAS report, “Medication Inventory Management 2019: How Close Is Your Vendor to Enabling True Enterprise MIM,” reveals Cerner and Epic’s MIM software ability to serve as an agnostic solution to manage inventory across disparate hardware is not a
Read More
Connecticut Launches State-Wide Hospital Quality Scorecard & Cost Estimator
The Connecticut Office of Health Strategy (OHS) has launched a state-wide online hospital quality scorecard and cost estimator solution called Healthcare CT to assist residents in making informed decisions concerning their healthcare among healthcare providers. The website has interactive tables and graphs that allow consumers to search, sort, and filter by entity, quality measure, health topic, and rating. In addition, the solution promotes cost transparency in healthcare improves access to
Read More
How A Hybrid Cloud Fax Solution Protects Patient Health Information
Electronic health and medical records (EHRs) enhance the patient experience and improve care coordination, but they can also put patients and providers at risk if they are not protected. Security vulnerabilities can arise from communicating via unsecured channels such as email and can result in data breaches, compromised patient records, and even identity theft. As medical records contain personal information such as social security numbers and insurance ID numbers, they are often even more
Read More
Cerner Launches Patient-Focused Wellness Communities for Seniors
Cerner is teaming up with LifeCenters, a planned wellness community development company, to provide primary care, pharmacy and fitness programs to senior-living communities across the country. Known as VIA Centers, residents will have access to primary care physicians and specialists including dieticians, chiropractors, fitness and health coaches at their Wellpoint properties. Through highly specialized care, the centers will engage patients and their health needs by focusing on diagnosing the
Read More
Genneve Raises $4M for Telemedicine Clinic for Women with Menopause
Genneve, a Seattle-based digital health company for women in midlife & menopause has raised $4M in seed funding led by BlueRun Ventures including participation from Maven Ventures and Startup Health. The latest round brings the startup’s total funding to date to $5.3 million, GeekWire first reports.Telemedicine Clinic for MenopauseEvery woman will experience menopause which lasts 4-10 years, costing her on average $20k through trial-and-error spending on prescriptions, doctor visits,
Read More
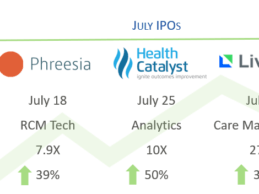
Research: July Digital Health IPOs, M&A Activity, Public Company Performance Summary
Summary of Health IT/digital IPOs, merger & acquisition (M&A) activity, and public company performance during the month of July.
Digital Health IPOs in July
Breaking the digital health IPO drought, there were four initial public offerings (IPOs) during a five-week period from late June to late July, including Livongo, Health Catalyst, Phreesia, and Change Healthcare. The last health IT companies to reach IPO were iRhythym Technologies and Tabula Rasa Healthcare in late 2016 -
Read More
NYC Health + Hospitals Launches Primary Care-Centered Diabetes Management Program
NYC Health + Hospitals, the largest public health care system in the nation announced the launch of a comprehensive, primary care-centered diabetes management program. The diabetes management program includes investing in new clinical pharmacy staff, equipment, and technology to improve health outcomes and expand services through telehealth techniques for more than 60,000 New Yorkers with diabetes who receive care in the City’s public hospitals and community-based health centers.Impact of
Read More