Never before has health informatics played a greater role in public health than during the COVID-19 pandemic. While the Health IT industry is certainly challenged due to the overall disruption to the healthcare system, the pandemic undoubtedly underscores the opportunity and importance of health informatics, such as telehealth, remote patient monitoring, patient engagement, AI-based drug discovery, precision medicine, and clinical decision support, but nowhere more pressing than the fields of bioinformatics, clinical surveillance, and predictive modeling.
One of the challenges that policymakers, public health officials, and economists are struggling to define is the true Infection Fatality Rate (IFR) of COVID-19. Case Fatality Rate (CFR) and Infection Fatality Rate (IFR) are often used interchangeably, but the definitions can be meaningfully different especially when there is the potential for a large discrepancy between Diagnosed and Infected cases, as is the case with COVID-19.
IFR = (Number of Deaths) / (Number of People Infected) x 100
CFR = (Number of Deaths / (Number of People Diagnosed) x 100
Farzad Mostashari shared a particularly insightful perspective via Twitter on April 17. Paraphrasing his thoughts, there are a few key considerations to make in using the case-rate curves to inform public policy.
1. The data we have today is based on report date, rather than date of symptom onset. In previous epidemics, like those for Salmonella, the lag between symptom onset and report date has been around 2-3 weeks. Such a lag creates potentially misleading trends – “Say you cleared a backlog of old samples last week, diagnosed a lot of old cases, it would look like a bump and then a decline.”
2. Rather than looking at a total number of cases, which can be skewed by testing volume, focus on the test positivity rate. During the week of 4/5 – 4/11, the overall positive rate was 21.4% and rising. This likely means we are still only testing people at high risk. Mostashari cited the very helpful CDC COVIDView Surveillance Summary.
3. The reported deaths are almost certainly undercounted. From March 11 to April 16, NYC recorded 9,447 non-COVID deaths in just over one month versus the normal of 5,400. Furthermore, it can take a month or more for patients to either recover or pass away, leading the death rate to significantly lag the case rate.
Farzad’s final assessment – “if we assume ~1% Case Fatality Rate (CFR) and 2,000 official deaths a day now –> 4,000 likely deaths a day –> we have been having 400,000 new cases a day not 30,000 […] we are undercounting cases by 10x+.” His interpretation undoubtedly underscores the complexity of information that we’re gathering on COVID-19.
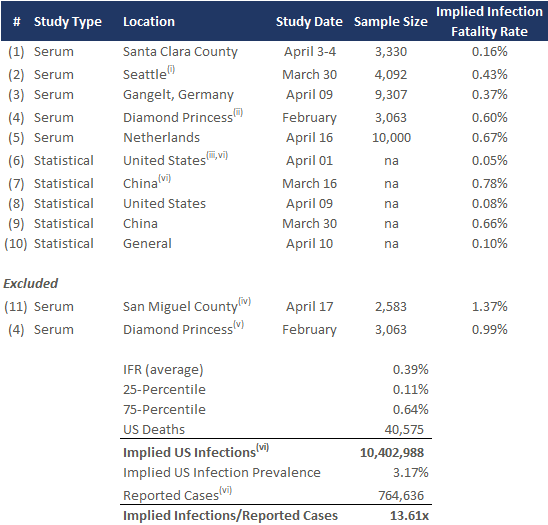
400,000 cases per day is significantly higher than the US reported case count of approximately 30,000 per day. Public health epidemiologists are working tirelessly to determine the actual prevalence and IFR of COVID-19, and three months into the pandemic, have yet to arrive at any consensus. In order to inform our readers, rather than take any opinion, we are summarizing key findings from various small-scale serum and statistical studies on the topic, which we’ve simply extrapolated against the US COVID-19 data as of April 18. Noting Dr. Mostashari’s comment that the number of deaths likely has a margin of error, we recognize the potential flaws of this extrapolation.
In the coming weeks, serum antibody tests will be completed at scale to measure the extent of both active and past infections, with dozens if not hundreds of such studies already underway worldwide. These tests will provide key data to model the course of the pandemic as well as inform the optimal public health and economic response, including gathering more data to address the still unvalidated question of the efficacy of antibody immunity itself (see the a study on the topic). Such data will also help epidemiologists determine IFR across age, gender, race, geography, and other sociodemographic factors that will inform the management of the disease and potentially the development and deployment of a vaccine.
Study Footnotes:
- (i) – # of infections as of March 15, midpoint of study date. Case fatality rate as of April 19, 2020.
- (ii) – Extrapolated Diamond Princess IFR to China population
- (iii) – Infection rate over a 3-week period
- (iv) – San Miguel has no fatalities, so we used Colorado mortality rate. Excluded due to small sample size in positive cases (only 17 positive cases so far in San Miguel county).
- (v) – Median age on ship 58, all 7 deaths 70+
- (vi) – Deaths and Reported Cases pulled from Worldometers data as of April 19, 2020.
Links to Studies:
- (1) – COVID-19 Antibody Seroprevalence in Santa Clara County, California
- (2) – Greater Seattle Coronavirus Assessment Network (Scan) Releases Data from First 18 Days of Testing, King County COVID-19 Data Dashboard
- (3) – Preliminary German Study Shows a COVID-19 Infection Fatality Rate of About 0.4 Percent, Worst-hit German district to become coronavirus ‘laboratory’
- (4) – Estimating the infection and case fatality ratio for coronavirus disease (COVID-19) using age-adjusted data from the outbreak on the Diamond Princess cruise ship, February 2020
- (5) – Dutch study suggests 3% of population may have coronavirus antibodies
- (6) – Using ILI surveillance to estimate state-specific case detection rates and forecast SARS-CoV-2 spread in the United States
- (7) – Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2)
- (8) – German study: U.S. only detecting 1.6% of COVID-19 cases
- (9) – Estimates of the severity of coronavirus disease 2019: a model-based analysis
- (10) – Robust Estimation of Infection Fatality Rates during the Early Phase of a Pandemic
- (11) – San Miguel County COVID-19 Information
Additional Helpful Resources:
- Coronavirus in the U.S.: Latest Map and Case Count
- Worldometer: COVID-19 Coronavirus Pandemic
- Why We Don’t Know the True Death Rate for Covid-19
- CDC launches studies to get more precise count of undetected Covid-19 cases
- MLB employees to be subjects of country’s largest COVID-19 antibody study
- @NateSilver538
- @Farzad_MD
Disclaimer: The information contained in this article is provided for informational purposes only, and should not be construed as advice on any subject matter. You should not act or refrain from acting on the basis of any of this content.
About Healthcare Growth Partners (HGP)
Healthcare Growth Partners (HGP) is a Houston, TX-based Investment Banking & Strategic Advisory firm exclusively focused on the transformational Health IT market. The firm provides Sell-Side Advisory, Buy-Side Advisory, Capital Advisory, and Pre-Transaction Growth Strategy services, functioning as the exclusive investment banking advisor to over 100 health IT transactions representing over $2 billion in value since 2007.
