The U.S. healthcare system is undergoing a major transformation, from many freestanding hospitals and individual practices to fewer large, integrated healthcare systems. One motivating factor is the promise of greater efficiencies when it comes to delivering more holistic patient care and improving core operational processes.Revenue cycle management is one process that’s primed for improvement. Poor billing practices can cost hospitals millions of dollars due to lost reimbursement or the
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
Revenue Cycle Startup AxiaMed Lands $12.4M for Patient Payment Platform
AxiaMed, a patient payment solution provider has raised $12.4 million in funding from Health Enterprise Partners. AxiaMed credits this investment to rapidly-increasing demand for its proven, secure, SaaS-based payment platform, Payment Fusion. Founded in 2015, AxiaMed’s integrated payments technology platform, Payment Fusion, improves the financial performance of healthcare providers through integration with various revenue cycle, practice management, EHRs and other software systems, enhancing
Read More
Patientco Lands $28M to Reimagine the Patient Financial Experience
Patientco latest Series B funding fuels expansion of patient billing and payments technology platform focused on creating a smarter patient financial experiencePatientco, an Atlanta, GA-based next-generation patient billing and payments technology company has raised $28 million in Series B funding led by private equity firm Accel-KKR. The round also included participation from BlueCross BlueShield Venture Partners / Sandbox Advantage Fund. Patientco plans to use the funding to accelerate expand
Read More
Apixio Unveils AI-Powered Risk Adjustment Auditing Solution for Plans & Providers
Apixio Inc., the data science company for healthcare, today announced availability of the first-ever AI-powered solution to help health plans and provider organizations to undertake internal audits of their risk adjustment payment data with increased accuracy and in far less time than traditional methods. Medicare is increasing the frequency of health plans audits offering Medicare Advantage (MA) products to ensure correct payments. Given the potential revenue impact, it typically takes health
Read More
8 Tips for Urgent Care Clinics to Optimize Revenue & Remain Profitable
As the 2017-18 flu season winds down, it’s become clear that it was one for the record books. With the onset coming early and strong, emergency departments, primary care physicians, and urgent care clinics all over the country were overrun with patients waiting in line to see a doctor.While this had a negative impact on a large portion of the U.S. population, anyone involved in the on-demand healthcare space knows that the flu season and resulting increase in patient volume tends to feed the
Read More
The Patient Experience and…Revenue Cycle Operations? The Two Are More Interlinked than You Might Think.
Think back to the last time you read a negative review about a restaurant. After reading the review, you probably dismissed the restaurant and considered other places to eat.Now, imagine you’re a patient considering options for an outpatient procedure and you came upon negative reviews about a provider. Chances are, you probably skipped that provider and opted for a consult with someone else. As providers, how can we fix this? Now, more than ever, patient satisfaction matters, especially given
Read More
Change Healthcare Launches Consumer Payment Solution to Transform Their Financial Experience
This week, Change Healthcare unveiled Member Healthcare Payments, a consumer payment solution that enables health plans to display consolidated patient financial information in a single destination, and empower consumers to better understand and manage their healthcare finances. Additionally, Member Healthcare Payments helps health plans better support providers by collecting patient payments, which can eliminate the provider's need to collect those payments.The first health plan to utilize
Read More
DrChrono EHR Integrates with Collectly to Automate Billing & Collections for Practices
DrChrono Inc., the company enabling the medical practice of the future, today announced a new partnership withCollectly, a fellow Y Combinator company that streamlines the billing and collection process for healthcare companies.Collectly digitizes paper bills and works with practices to send patient billing statements and collection notices electronically via text or email. Within the message is a link for patients to go straight to a patient portal to see their statement and instantly make a
Read More
Report: Healthcare Organizations are Seeing Improved Profits from Value-based Care Contracts
46% of healthcare organizations see value-based care contracts improving profitability versus 23% two years ago. Healthcare organizations are more optimistic about how value-based care will affect their finances, according to a poll of accounting and finance employees on a webcast that KPMG hosted. Government spending on healthcare through Medicare, Medicaid, Veterans Administration and other programs have been shifting to value-based payment models in an attempt to improve efficiency and tie
Read More
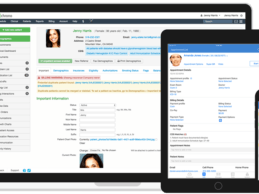
Solving the Patient Access Labor Supply Challenge
Providers are struggling to stay profitable while also striving to keep patient satisfaction from being negatively impacted. Denials are on an upward trend, payors are becoming tighter around what is demanded of the providers, and patients are being squeezed to pay more out-of-pocket with the ongoing shift to self-pay and high-deductible plans.What many may not realize is that these financial challenges rear their head from the moment the patient walks through the door or schedules an
Read More