The evolution of e-commerce – led by Amazon – has created an intensely savvy consumer population. Amazon’s platform allows users to easily compare products from different vendors to get the best price. People travel to retail stores to try on clothes and shoes, only to purchase them online for less. Even the longest running game show in television history awards points for knowing how much consumer products cost.
Healthcare, on the other hand, does not engender the same kind of
Read More
Prior Authorization
Prior Authorization Reforms Don’t Address the Real Problem. Here’s How AI Can Help.
After waiting weeks for an open appointment, John finally gets in to see the orthopedic surgeon to evaluate his acute knee pain. He’s already been off work for over two months and has barely been able to leave the house, popping anti-inflammatory and pain medicine to manage the pain every day.
Suspecting a torn meniscus, the doctor orders an MRI to verify the diagnosis and plan his treatment approach. The nurse begins the process by calling John’s insurance carrier to verify coverage,
Read More
AdvancedMD to Roll Out 35+ Updates in Major Product Release
What You Should Know:
- AdvancedMD announced its 2022 Fall product release that includes 35 new features added to its suite of all-in-one medical office and remote care cloud software. This marks one of the largest product release updates in AdvancedMD history, reflecting the robust nature of the leading cloud-based platform used by more than 40,000 practitioners across 13,000 practices, and 850 medical billing companies.
- AdvancedMD’s fall release ensures more unified and smoother
Read More
HLTH22 Day 3 News Summary
DispatchHealth Raises $330M for Hospital-at-Home Care
DispatchHealth, a provider of in-home medical care raises $330M led by Optum Ventures with support from current investors such as Humana (NYSE: HUM), Oak HC/FT, Echo Health Ventures and Questa Capital. New investors included Adams Street Partners, the Olayan Group, Silicon Valley Bank, Pegasus Tech Ventures and Blue Shield of California. Patients and their care partners can request DispatchHealth medical care via phone, mobile app, or
Read More
Edifecs Partners with Empowered-Home to Deliver Automated Prior Authorizations
What You Should Know:
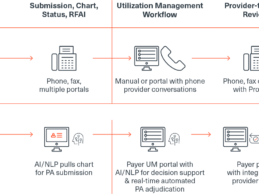
- Edifecs and Empowered-Home announced a partnership to provide automated prior authorizations to medical associations, Accountable Care Organizations (ACOs), Independent Physician Associations (IPAs), medical groups, and home health care agencies.
- The Edifecs prior authorization solution combined with the clinical decision support system of patient management software company, Privis Health, forms the backbone of Empowered-Home’s ecosystem. Empowered-Home is
Read More
Notable Survey: 61% of Patients Skip Medical Appointments, Due to Scheduling Hassles
What You Should Know:
- Notable, the leading intelligent automation company for healthcare, today announced the results of a new patient survey, highlighting that legacy digital solutions and manual workflows limit patients’ ability to access care.
- 61% of patients surveyed said that they skipped going to the doctor in the past year because scheduling an appointment was too much of a hassle.
Evaluating Why Patient Portals Fail to Meaningfully Expand Access to Care
Notable is
Read More
3 Questions Healthcare IT Leaders Should Ask Before Implementing AI in Their Operations
Artificial intelligence (AI) and automation are no longer nice-to-have technologies for healthcare providers. They are mission-critical tools for addressing significant challenges many health systems and hospitals face today — from volatile patient volumes to ballooning labor costs and staffing shortages to low operating margins. Many of these challenges are macro-level economic trends that will continue to prevail for the foreseeable future.
According to research from Kaufman Hall,
Read More
Humana Taps Cohere Health to Streamline Prior Authorizations for Cardiovascular & Surgical Specialties
What You Should Know:
- Health insurer Humana has expanded its partnership with Cohere Health to streamline the prior authorization process for cardiovascular care and surgical specialties. Both these care pathways are clinically complex, involving multiple exchanges between primary care physicians and specialists, which can contribute to costly and unnecessary variations in care.
- For surgical services, Humana staff will use the Cohere Unify™
Read More
Why Data is at the Heart of Value-Based Care Success
The saying “you cannot manage what you cannot measure” applies to all aspects of healthcare delivery, but it is especially true in value-based care. After all, payers, providers, and the patients they care for need to know what high-value care looks like at an individual level – and how it can be applied at the population level.
Delivery and technology infrastructure. All too often, data is captured in disparate systems, forcing administrative staff – or, worse, physicians and nurses – to
Read More
Top Job Stressors for Pharmacist and Prescribers, Exacerbated by Incomplete Patient Data
What You Should Know:
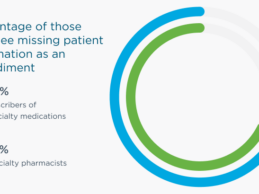
- Survey data released by Surescripts, a health information network, showed that two-thirds (65%) of specialty prescribers and almost three-quarters (73%) of specialty pharmacists agree that the leading cause of delays in getting patients started on their specialty medications is due to issues often caused by outdated processes and paperwork required for prior authorization.
- The survey, taken this summer by 501 specialty pharmacists and prescribers of specialty
Read More