What You Should Know:
– Edifecs and Empowered-Home announced a partnership to provide automated prior authorizations to medical associations, Accountable Care Organizations (ACOs), Independent Physician Associations (IPAs), medical groups, and home health care agencies.
– The Edifecs prior authorization solution combined with the clinical decision support system of patient management software company, Privis Health, forms the backbone of Empowered-Home’s ecosystem. Empowered-Home is connected with medical associations in multiple states including New York, Texas, Washington, Montana, and Hawaii because it is a complex ecosystem that requires cooperation from both sides.
Why this Matters
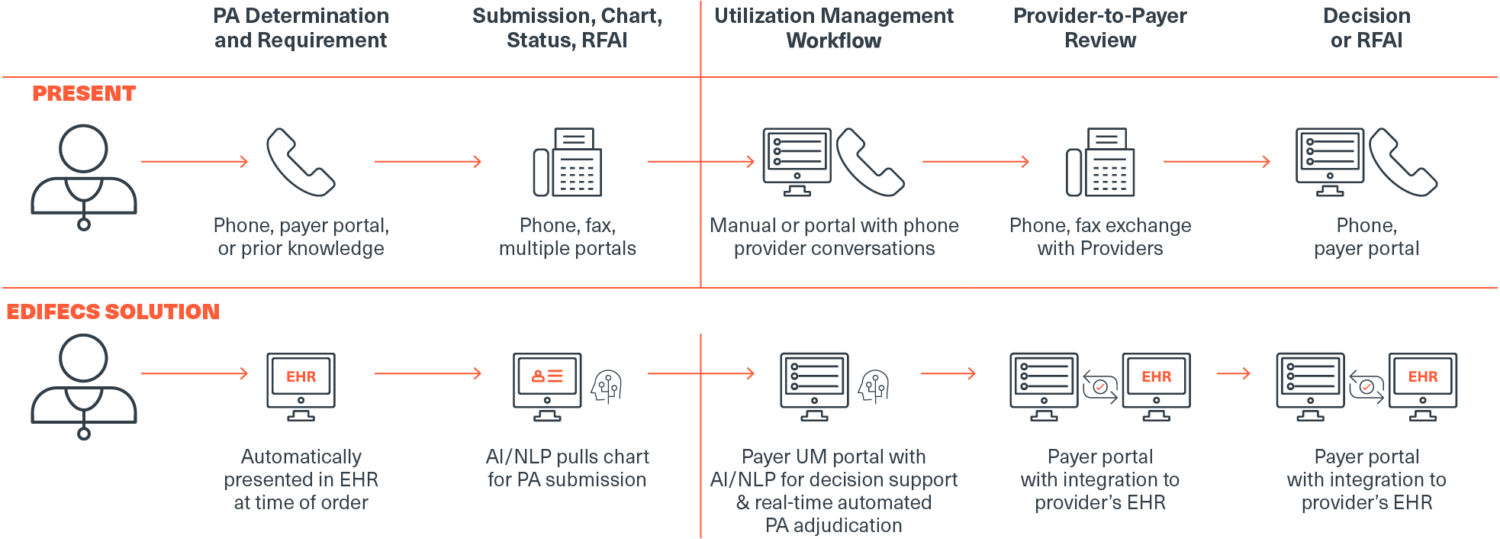
The burden of the prior authorization process is approximately 16 hours per week or $80,000 per ordering physician per year. The delay in treatment is often over 30 days and can cause a significant detriment to the care regime and patient health. The Edifecs prior authorization solution provides real-time adjudication resulting in more accurate billing, fewer claim denials, and faster reimbursement. Additionally, it significantly decreases the administrative burden on providers allowing them to focus more time on patient care and alleviate physician burnout.
“As strong supporters of the ‘Improving Seniors’ Timely Access to Care Act,’ we are proud to be partnering with Empowered-Home to automate the prior authorization process for its customers and partners, and ultimately provide seniors with more timely access to care,” said Venkat Kavarthapu, CEO of Edifecs. “The prior authorization process is cumbersome and costly for both payers and clinicians. We have worked hard to alleviate that burden by automating it from the provider’s EHR system to the payer’s utilization management workflow.”
