Intermountain Healthcare has formed a new comprehensive health platform company named Castell that will enable other organizations to accelerate their transition from volume to value-based systems of care, while keeping care more affordable and accessible. Rajesh Shrestha has been named as the president and CEO of Castell. In addition to leading Castell, Shrestha serves as vice president and chief operating officer of Community Based Care for Intermountain Healthcare. He has more than two
Read More
Medicare Insurance| Regulatory, Policy, Patients Analysis, Insights - HIT Consultant
Why Coworking Spaces Are Essential for Medical Practices
Collaborative work environments remain one of the biggest trends in office space. These coworking spaces have proven to improve the happiness, productiveness, and well-being of employees. However, the use of coworking spaces remains greatly underdeveloped in a medical industry that has seen private practice rates plummet in recent years.
For many physicians, having a private practice is the optimal professional scenario. And yet, private practices are in steep decline. In 2016, less than half of
Read More
ACO Investment Model Reduced CMS Expenditures by $48M
The Accountable Care Organization (ACO) Investment Model (AIM) saved the Centers for Medicare & Medicaid Services (CMS) more than $48M in its first year while promoting improved health care in rural and underserved areas, according to a new study from Abt Associates.The new study reveals that after accounting for the $82.4 million provided to ACOs, AIM reduced CMS expenditures by $48.6 million. Decreases in the number of hospitalizations and use of institutional post-acute care contributed
Read More
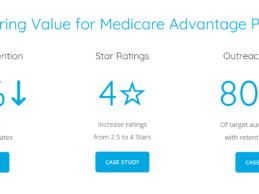
How Medicare Advantage Plans Reduced Their Disenrollment Rates by 30% Through Welltok
The average Medicare Advantage plan turns over about 10% of its members every year, and for a 100,000 member plan, that can equate to about $110 million in lost premium reimbursements as well as a decline in Star ratings. This is why retaining members is a top priority among health plans. Welltok’s Medicare Retention Solution has helped leading Medicare plans reduce disenrollment rates by up to 30%, improve disenrollment-related Star ratings from 2.5 to 4 and retain up to $97 million
Read More
6 Considerations For Creating A Robust Healthcare Data Analytics Program
Healthcare organizations are increasingly turning to data analytics to solve their toughest business challenges. As information becomes less siloed, and technology systems do a better job of both generating and sharing data, organizations are seeing the need to more precisely identify patterns to predict patient needs, anticipate resources and improve processes. There is now as much emphasis on making the data work as there was on collecting data, so it can affect change.
Unfortunately,
Read More
Innovaccer Launches Data Solution to Enable ACOs’ Seamless Transition to Value-Based Care
A survey suggests that 71% of accountable care organizations would rather quit the Medicare Shared Savings Program than assume down risks. Although ACOs are leading the transition from volume-based care to value-based care, a lot of them face the lack of confidence in meeting the quality and cost benchmarks. When ACOs don’t have adequate knowledge and control over the network, earning shared savings can be quite challenging. Data from disparate sources such as EHRs, payer claims, PMS and HIEs
Read More
Pilot Study: Lark Health’s AI-Driven Diabetes Management Program Decreased A1c by 1.1 Points
Lark Health, a chronic disease prevention and management platform has released initial results from a pilot study of its Diabetes Management Program (Lark DMP). After an average of four months, the Lark DMP users reported a significant reduction in A1c levels of 1.1 points, from 8.5 to 7.4 percent.Lark Diabetes Management Program OverviewThe Lark DMP, which uses conversational artificial intelligence (AI), rather than live telephonic nurses, was developed with the collaboration of industry and
Read More
Carenet Health Acquires Engagement, Telehealth Subsidiary of Citra Health
Carenet Health, a San Antonio, TX-based provider of healthcare engagement, clinical support, advocacy and 24/7 telehealth solutions, has acquired the engagement and telehealth solution subsidiary of Citra Health Solutions. The acquisition is the second acquisition of its kind by Carenet in a span of seven months. Financial terms of the acquisition were not disclosed.The recent acquisition complements Carenet’s ongoing commitment to delivering high-quality, cost-effective, on-demand telehealth
Read More
AMA Grants New CPT Code for KidneyIntelX to Support Medicare & Reimbursement
The American Medical Association (AMA) has granted a CPT® Proprietary Laboratory Analyses (PLA) Code for Renayltix AI’s lead product, KidneyIntelX. The new code, 0105U, has been approved and published by the AMA CPT Editorial Panel, and is scheduled to become effective on October 1, 2019.Medicare Price for New CPT CodeA payment rate for the new code will be established for Medicare patients through the 2019 Clinical Lab Fee Schedule (CLFS) Annual Public Meeting process. Renayltix AI will shortly
Read More
How Can Providers Support Meaningful Price Transparency to Address Consumerism in Healthcare?
The word “consumerism” and its derivatives have been tossed around the broader healthcare industry for the greater part of a decade. How we define consumerism and look at consumer behavior in relation to our institutions, systems, and programs seems key to unlocking the door to better outcomes and higher margins. However, in a landscape with more disruption than ever—greater vertical integration, technology, and regulation—we still lack the answer to these fundamental questions: What do patients
Read More