Virtual care is everywhere and ubiquitous. But at a time when the world is amid a global pandemic, virtual care is also being underutilized. The technology exists today to help our healthcare system not only more effectively and efficiently manage care during COVID-19, but also exponentially scale capacity in the face of future outbreaks.
Virtual care defined
Virtual care is a broad term. It encompasses all the ways healthcare practitioners provide for care remotely. This can mean video visits or secure text conversations with a doctor or nurse practitioner — essentially any way care teams remotely communicate with patients. It is also used interchangeably with telehealth, telemedicine, or digital health, and it’s becoming the norm.
Patient adoption of virtual at the beginning of 2020 was up 33% over the previous year, while funding has been booming and the market is expected to reach $185.6 billion by 2026.
In one recent survey, 80% of patients reported it very easy to schedule a virtual care visit, 77% were completely satisfied with the virtual care experience, and 70% were very likely to recommend the experience to others. Another report by Accenture confirms that globally, patients have embraced virtual care and want to see it continue post-pandemic. Nine out of ten patients indicate that the quality of care is as good or better than it was before. They see virtual care as more time-efficient. And they believe the use of technology has allowed healthcare providers to maintain or improve the patient experience.
So while face-to-face visits are still essential in some cases, for most scenarios, there is a growing general agreement amongst consumers of healthcare that virtual visits will suffice for many of the scenarios where we interface with the healthcare system.
The barriers to adoption begin to fall
In the United States with CMS, both Medicare and Medicaid now have codes that allow practitioners and institutions to get reimbursed for virtual care. This opening up of the economic pathways coupled with new care constraints created by the pandemic has accelerated virtual care adoption.
According to the American Medical Association, physicians and other health professionals are now seeing 50 to 175 times the number of patients via telehealth than they did before the pandemic. The report notes that 46% of patients are now using telehealth to replace canceled in-person visits, up from just 11% of patients who used telehealth in 2019.
The dams are breaking down to allow for an exponential increase in the uptake of virtual care. When you look at the healthcare ecosystem in the United States, patients, clinicians, payers, manufacturers, and distributors are now on board. So for the consumer or provider who is interested in delivering this level of care, there should be no barriers. There are lots of choices. There’s lots of access. And doctors will be more than adequately reimbursed for these services.
COVID-19 builds a strong case for digital healthcare delivery
So how can virtual care help us with COVID-19? By way of example, I’d like to share the story of a doctor friend of mine, Rick. He was recently isolated because of an exposure he had to a COVID+ individual. He’s a very active physician in his community. While in isolation, he was able to provide continued care to his patients using video conferencing. He’s still being compensated for his time. He’s conducting business as usual and still managing to put a dent in the pandemic without ever leaving his home. That’s just one illustration of the power of virtual care from a pandemic perspective. Virtual care can also be used to screen out those patients who are worried or ill. Technologies can be used to remotely monitor those with a suspected or proven infection. We can provide care to other patients who have nothing to do with COVID-19, but who need ongoing care because of their chronic conditions. And, most importantly we can minimize our exposure as healthcare workers. We’re a limited resource due to COVID-19 and virtual care allows us a pathway to safely continue to serve those in need.
When you think about how virtual care is being used during the pandemic to screen out patients and to provide care, I’d argue it is better than before. So, why then, with all the tools available to us are we still resorting to parking lot pop-up screening clinics with hours-long line ups and paper charts versus digital surveys? You can only imagine the emotional stress and toll this is having not just on those waiting, but the health care teams doing the screening.
There is a better way to deliver these services. And I would argue that it’s virtual. It’s safer for both the practitioner and the patient. For instance, what if we have a community outbreak and public health would like to conduct a mass survey of the community. By using a digital survey, people can access it to screen themselves. If they are self-isolating or quarantining, they can monitor their symptoms. From the digital information gathered, public health can identify those who should go on to have further screening, or perhaps a nasopharyngeal swab. It can be used for assessment and triage, and in combination with plug-and-play Bluetooth devices, vital signs information such as temperature can be automatically collected. Processes can be automated so should patients meet a certain threshold, caregivers can be notified to trigger screening or hospitalization.
Just imagine the burden this would take off the healthcare system if we were to do all this remotely using existing digital technologies and cloud-based systems. In this scenario, a physician such as myself could manage hundreds of patients from the comfort of my own home or in my clinic without seeing them face to face. I’d be able to instantly identify those needing further action, whether that is an email, a video visit, a message, or an alert that they should go to a hospital immediately.
Emerging technologies can unlock improved care delivery and greater efficiencies
In the not too distant future, new technologies will emerge (likely at an accelerated rate given that the pace of innovation speeds up when necessity is the driver) that will be hugely beneficial in a future pandemic.
Imagine a smartphone app that allows doctors to screen people with coughs and classify a normal cough from one that is based on a diseased state. It could be used for mass screening and perhaps even diagnosis of a respiratory illness. This technology is being tested as we speak to verify people with active tuberculosis in Africa.
Imagine a technology that uses artificial intelligence to scan the Internet for information to help early identification of outbreaks. It exists today and the startup behind it was the first organization on the planet to identify the Wuhan outbreak — before the WHO was even aware of it using its conventional news and big data tracking.
And imagine a wearable that can continuously track and measure a person’s critical vitals including their blood pressure on a beat to beat basis, heart rate, ECG, breathing rate, positional information, oxygen levels, and temperature, all in real-time, with information streamed to the cloud and into the hands of caregivers, instantly alerting them should a condition deteriorate. For the average person, this may be overkill. But for someone with COVID-19 sent from the hospital to recover at home, or for another patient that is at high risk, this technology could be a lifesaver.
It’s just about great care.
Virtual care is not something extraordinary or special. It’s just care. Those of us who have now digitally intersected with the healthcare system, whether through an app, or a video visit, or an email or text, would likely agree with me.
Virtual care is hugely beneficial during a pandemic. It’s safe, efficient, and accessible, and most certainly better than the pop-up drive-through screening clinics we’re seeing in parking lots across North America.
If there is one big sticking point, it is that we are under-utilizing virtual care. In this time of need, administrators are acting too slowly and in a way that is not best-suited to society’s needs. Virtual care is safer, more efficient, and less costly. And with some of the new technologies on the horizon, can be useful for earlier detection, earlier intervention, and better care during future outbreaks and during normal non-pandemic times.
About Dr. Kohli’s
Dr. Sonny Kohli is a practicing Physician in Internal Medicine and Critical Care and is Faculty at SingularityU Canada as well as McMaster University. In 2008/09, Sonny was a top 40 Astronaut Candidate in the Canadian Space Agency (CSA) recruitment campaign. He is also an alumnus of the International Space University, a trained flight surgeon with the Canadian Forces, and was awarded a CSA scholarship to Johnson Space Center & Wyle Labs. While studying at ISU, he helped deploy the Image Reversal In Space (IRIS) experiment on the International Space Station.
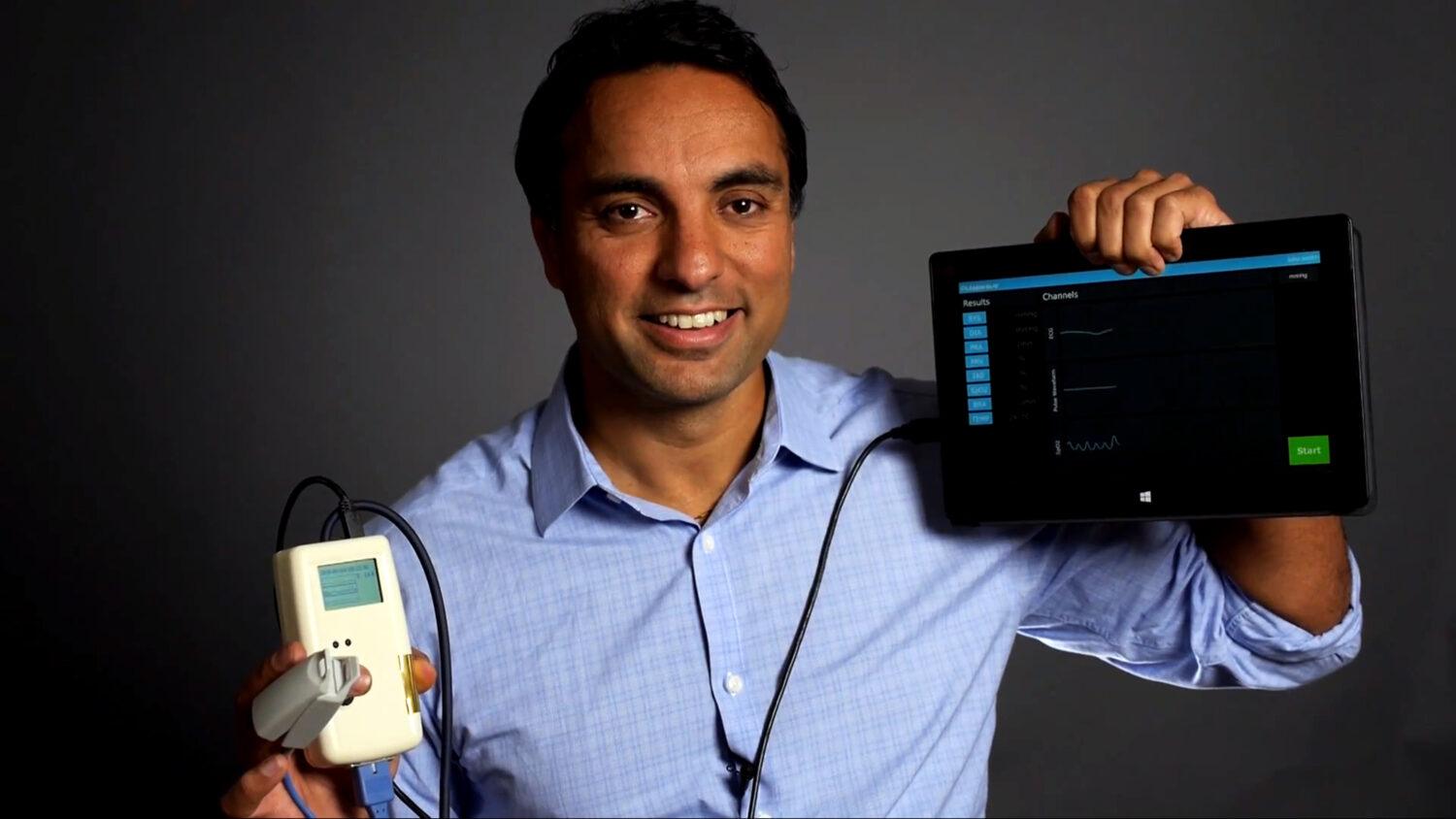
In 2010, while volunteering in post-earthquake Haiti, Sonny experienced first-hand the perils of inadequate health care faced by Earth’s most marginalized peoples. Intrigued by space-age and digital solutions to the world’s health problems, Sonny co-founded Cloud DX to create a fully autonomous ‘digital doctor’ called Vitaliti. Sonny and Cloud DX were bestowed as XPRIZE’s first ever ‘Bold Epic Innovator’ as part of the Qualcomm Tricorder XPRIZE competition.
