As healthcare finance leaders prepare to gather for the upcoming HFMA Annual Conference, they face a familiar but intensified set of challenges: shrinking margins, rising operational costs, and an increasingly complex reimbursement landscape. This year, however, a dominant theme emerges from the conversation: the role of Artificial Intelligence in revolutionizing the revenue cycle. We asked six healthcare executives for insights on what key themes/trends they expect to be the most talked
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
How Cyber Threats Are Reshaping Healthcare Revenue Cycle Strategy
The impact of any data breach cannot be overstated, especially in healthcare. Unlike other sectors, such as financial services or travel, healthcare records contain “one of one” data – medical history cannot simply be replaced or revoked, making this data uniquely valuable to threat actors.
Unfortunately, healthcare has seen a clear surge in data breaches in recent years.
Financially motivated hackers and insider threats are increasingly exploiting cybersecurity gaps that were
Read More
Humata Health’s AI-Powered Prior Authorization Platform Now Available on Microsoft Azure Marketplace
What You Should Know:
- Humata Health, a provider of AI-powered touchless prior authorizations, today announced the availability of its platform in the Microsoft Azure Marketplace, an online store providing applications and services for use on Azure.
- The integration allows healthcare payers and providers seeking to automate prior authorization to leverage the productive and trusted Azure cloud platform, with streamlined deployment and management.
Transforming End-to-End
Read More
85% of Cancer Patients Face Unnecessary Insurance “Red Tape” Due to Prior Authorization, Says New CancerCare Report
What You Should Know:
- A new national survey from CancerCare reveals how insurance utilization management practices, particularly prior authorization, create serious and stressful barriers to care for cancer patients. The report, titled "The Health Insurance Maze: How Cancer Patients Get Lost in the Red Tape of Utilization Management," found that these requirements frequently delay diagnosis and treatment, adding significant "time toxicity" to patients' lives.
- The
Read More
Scalability in Revenue Cycle: Building a Flexible Model for Sustainable Growth
The demands on revenue cycle management (RCM) today are unrelenting. Healthcare providers are navigating ongoing regulatory shifts while financial constraints and growing patient volumes place immense pressure. The average internal cost of running an RCM operation has increased from 4% to 5%, even with the advances in technology and automation. To be successful, providers must maintain efficiency while delivering quality care.
With this current landscape, RCM must be built for adaptability;
Read More
Smarter Technologies Launches AI-Driven Platform to Tackle Hospital RCM Inefficiencies
What You Should Know:
- Smarter Technologies, an automation and insights platform focused on healthcare efficiency, announced its official launch.
- The new company brings together the strengths of Access Healthcare, SmarterDx, and Thoughtful.ai, three entities that recently received strategic growth investments from New Mountain Capital, LLC, a growth investment firm with over $55B in assets under management.
- Smarter Technologies debuts as the industry’s first
Read More
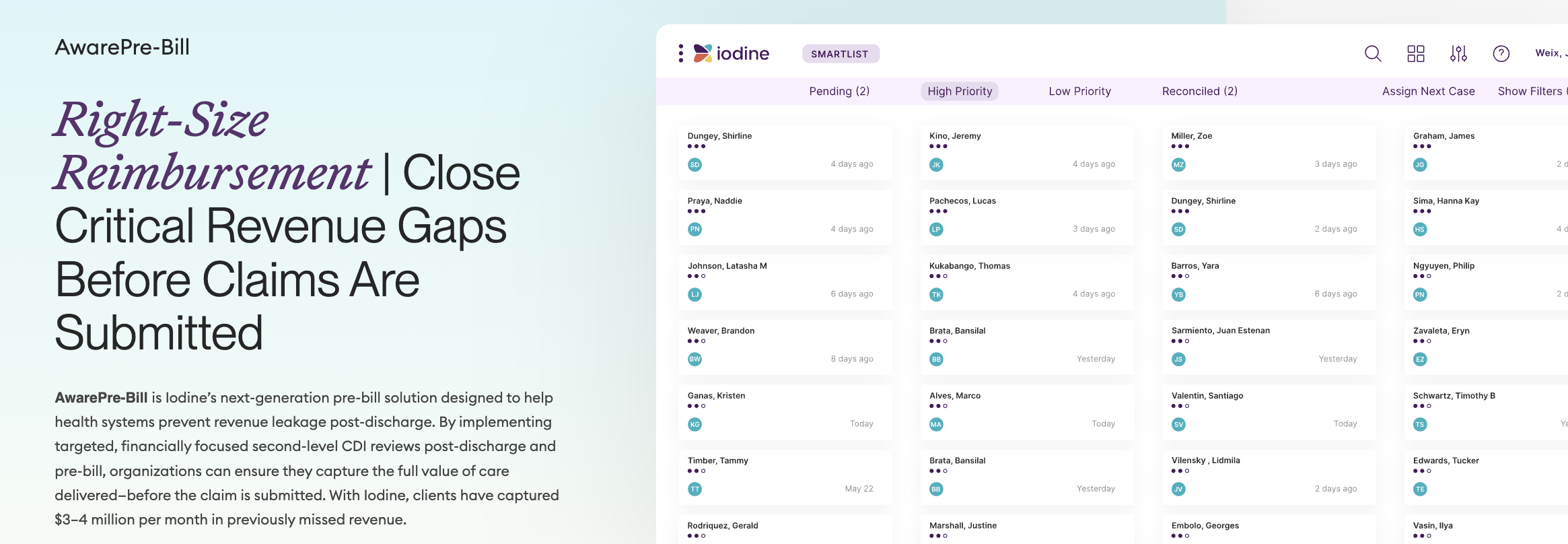
Iodine Software Launches Next-Gen Pre-Bill Solution
What You Should Know:
- Iodine Software, the leader in healthcare AI for revenue cycle optimization, today launched the next generation of its pre-bill solution, AwarePre-Bill, designed to help health systems close critical revenue gaps before claims are submitted.
- Built on years of proven success, the solution enables health systems to conduct financially targeted retrospective reviews, improving code accuracy and documentation to help right-size reimbursement. With Iodine, clients
Read More
IKS Health and GI Alliance Partner to Optimize Gastroenterology RCM and Clinical Efficiency
What You Should Know:
- IKS Health, a global leader in care enablement solutions designed to support clinicians, staff, and patients throughout the care journey announced a significant partnership with GI Alliance, the largest independent gastroenterology (GI) services organization in the United States.
- The collaboration aims to deploy advanced AI-enabled technology and human intelligence to create a best-in-class revenue cycle management (RCM) process specifically tailored
Read More
Infinx Acquires i3 Verticals’ Healthcare Revenue Cycle Management Business
What You Should Know:
- Infinx Healthcare, a leading provider of AI-powered solutions for patient access and revenue cycle management (RCM), today announced it has acquired the Healthcare Revenue Cycle Management Business of i3 Verticals, Inc. (NASDAQ: IIIV).
- The transaction strengthens Infinx’s market presence in the healthcare RCM space and expands its footprint into new customer segments, including academic medical centers and other large provider groups.
Infinx Enhances AI-Driven
Read More
Cedar Launches ‘Kora’ AI Voice Agent to Automate Patient Billing Calls
What You Should Know:
- Cedar, a patient financial platform for healthcare providers announced the launch of Kora, its advanced AI voice agent designed to automate patient billing calls.
- Developed in collaboration with communications platform Twilio and already being implemented at leading providers such as ApolloMD, Kora leverages Cedar's deep healthcare expertise and proprietary billing data to deliver efficient and empathetic call resolution at scale.
Kora: An AI Voice
Read More