What You Should Know:
- Salesforce today announced new Customer 360 for Health capabilities that help healthcare providers deliver more personalized patient experiences and reduce operational costs.
- Customer 360 for Health helps healthcare and life sciences organizations enhance the overall care experience with the full power of Salesforce technology, including real-time data from Data Cloud, Einstein AI, and automation with Flow.
New Customer for
Read More
Prior Authorization
How Search Makes Clinical Natural Language Processing Useful in the Real World
Clinical Natural Language Understanding (cNLU), the technology by which computers extract meaning from clinical text, is quickly becoming a common feature in the healthcare IT landscape. In 2021, 30% of surveyed healthcare organizations were either using or exploring the technology. (Gradient Flow, 2021). Similar adoption is occurring in the UK as well. (Wu et. al, Nature, 2022). Today, cNLU is being applied to billing/coding, trial enrollment, registry creation, clinical decision support,
Read More
17 Execs Share How Health IT Can Address Clinician Burnout, Staffing, & Capacity
Clinician shortage has reached a new level of urgency as we face rising demand and healthcare costs, according to a recent Accenture report. Healthcare workers are increasingly burned out and leaving the industry altogether in droves. Those who remain to do the work are overburdened. We ask seventeen healthcare IT executives for their insights on how health IT solutions could potentially help address clinician burnout, clinician staffing shortages, and deal with capacity.
Staffing levels
Read More
A New Way of Thinking About Interoperability in 2023
Interoperability in the U.S. healthcare system has been an ongoing challenge. While there are several industry initiatives that are going to advance the industry and make incremental progress toward interoperability, there remain several gaps that are unaddressed.
Interoperability is a much broader concept that encompasses more than protocols, APIs, and limited networks. It’s about more than exchanging data through one-to-one connections between a provider, payer, or vendor. True
Read More
AGS Acquires Offshore Patient Access BPO Unit from Availity
What You Should Know:
- AGS Health, a provider for tech-enabled revenue cycle management (RCM) solutions announces the acquisition of the India-based patient access outsourcing business unit of the Florida-based healthcare technology company Availity.
- With more than half of U.S. hospitals anticipating a year of negative margins, achieving full and accurate reimbursement for services has never been more critical. With this expansion, AGS Health is positioned to provide faster, more
Read More
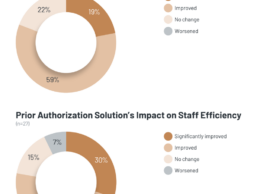
KLAS: What Impact Do Automated Prior Authorization Solutions Provide?
What You Should Know:
- Prior authorization is mandated by payers to ensure that certain clinical procedures and medications being ordered are necessary. To alleviate the heavy administrative burden this requirement causes, healthcare organizations have adopted automated prior authorization solutions.
- For this report, KLAS interviewed 30 respondents from 26 unique organizations to understand their experiences using these solutions and what outcomes they have seen.
Understanding
Read More
Why It’s Time for Intelligent Prior Authorization
The Centers for Medicare & Medicaid Services (CMS) recently proposed a new rule to advance interoperability and improve the prior authorization (PA) process for Medicare and Medicaid patients. Specifically, the rule stipulates that health plans adopt electronic prior authorization processes, adhere to shorter turnaround times, clearly communicate denial reasons, publish key metrics annually, and implement the Fast Healthcare Interoperability Resources (FHIR) Application Programming Interface
Read More
Electronic Transactions Can Benefit Partnership Among Physicians, Insurers and TPAs
The patient is at the center of the healthcare experience, and rightfully so. However, a strong case can be made to place the physician at the center. After all, it’s the physician who diagnoses and treats the patient.
Insurance companies and third-party administrators (TPAs) also have critical roles to play in the care experience, bringing together networks of physicians, specialists, surgery centers, hospitals, ambulatory care centers, and more to create a comprehensive care experience for
Read More
Edifecs and VirtualHealth Partner to Automate Prior Authorization
What You Should Know:
- Today, Edifecs and VirtualHealth, a medical management company, announced a new partnership automated prior authorization to VirtualHealth’s HELIOS® platform for healthcare payer and provider clients.
- The Edifecs solution will automate and optimize the prior authorization process across HELIOS to significantly reduce the administrative burden, alleviate friction between payers and providers, and ultimately expedite patient care.
Growing Need for Automated Prior
Read More
9 Executive Revenue Cycle Predictions/Trends to Watch in 2023
Nate Maslak, the co-founder/CEO of Ribbon Health
Price Transparency: In 2022, we saw CMS’s Transparency in Coverage rule go into effect, requiring non-hospital entities like health plans and providers to publish publicly available rates for care. In 2023, we’ll see this price transparency data become more mainstream as it finally makes its way into the hands of patients, empowering them to find the best care for them, reevaluate their care choices, and shop around for the best possible care
Read More