In the US alone, an estimated 1.9 million new cases of cancer were diagnosed in 2022, positioning oncology as a key subject of clinical research. Throughout oncology trial development, it is important that stakeholders acknowledge that only patients can fully understand the impact of treatment on their lives. Regulators are now looking beyond clinical indications such as tumor size and delayed disease progression. When evaluating the risks and benefits of treatment, they want to know whether the
Read More
Payers| Payer Industry Impact for Patients, Clinicians, and Healthcare Organizations | News, Analysis, Insights - HIT Consultant
From Telemedicine to Complete Virtual Care and Beyond
Telemedicine has helped improve the quality of life of patients in every corner of the world and has been successfully utilized to provide convenient care to people with limited or no access to health services. Today, worldwide digital interconnectivity is growing, enabling telehealth to advance health equity, bring access to care for underserved regions and meet the urgent, primary and behavioral healthcare needs of an exploding global population.
It has been a remarkable journey for the
Read More
Experian Health Launches AI-Driven Predictive Denials Management
What You Should Know:
- Experian Health launches a new AI-Powered solution, AI Advantage that will help providers recoup the billions in lost dollars due to insurance claim denials.
- These new solutions leverage AI and help healthcare providers prioritize their claims reimbursement process and decrease denials overall, saving time and money across the entire healthcare value chain and ultimately improving care and service for patient consumers.
AI Advantage
One of the top
Read More
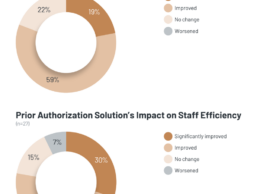
KLAS: What Impact Do Automated Prior Authorization Solutions Provide?
What You Should Know:
- Prior authorization is mandated by payers to ensure that certain clinical procedures and medications being ordered are necessary. To alleviate the heavy administrative burden this requirement causes, healthcare organizations have adopted automated prior authorization solutions.
- For this report, KLAS interviewed 30 respondents from 26 unique organizations to understand their experiences using these solutions and what outcomes they have seen.
Understanding
Read More
Why It’s Time for Intelligent Prior Authorization
The Centers for Medicare & Medicaid Services (CMS) recently proposed a new rule to advance interoperability and improve the prior authorization (PA) process for Medicare and Medicaid patients. Specifically, the rule stipulates that health plans adopt electronic prior authorization processes, adhere to shorter turnaround times, clearly communicate denial reasons, publish key metrics annually, and implement the Fast Healthcare Interoperability Resources (FHIR) Application Programming Interface
Read More
FHIR Adoption and Implementation Challenges
The Fast Healthcare Interoperability Resources (FHIR) standard was introduced by HL7 in 2014 as a significant replacement for the HL7 V2 and V3 standards. An open standard called FHIR, which was initially drafted in 2011 makes it easier than ever for legacy systems and new apps to exchange data. FHIR was created to not only increase communication efficiency and interoperability compared to earlier standards but also to facilitate implementation by giving clear specifications and allowing
Read More
Faro Health Secures $20M to Streamline Smart Clinical Trials
What You Should Know:
- Faro Health, a cloud-computing company that is developing digital infrastructure for smart clinical trials raises $20M in Series A funding led by General Catalyst to help scale the digital transformation of clinical trials––essentially making it easier and quicker for drug developers to greatly reduce the cost and time of trials.
- The round also included participation from previous investors Section 32, Polaris Partners, Zetta Ventures, and Northpond Ventures.
Read More
Ushur Lands $50M for Customer Experience Automation Platform
View ClaimsView Claim
What You Should Know:
- Ushur, the leader in AI-powered Customer Experience Automation™ (CXA), has raised a $50M Series C funding round led by Third Point Ventures with participation from existing investors Iron Pillar, 8VC, Aflac Ventures and Pentland Ventures.
The company plans to use the funding to expand Ushur’s experience automation portfolio, developing new innovations in AI and moving into new regions and industry verticals.
Healthcare Automation
Read More
Electronic Transactions Can Benefit Partnership Among Physicians, Insurers and TPAs
The patient is at the center of the healthcare experience, and rightfully so. However, a strong case can be made to place the physician at the center. After all, it’s the physician who diagnoses and treats the patient.
Insurance companies and third-party administrators (TPAs) also have critical roles to play in the care experience, bringing together networks of physicians, specialists, surgery centers, hospitals, ambulatory care centers, and more to create a comprehensive care experience for
Read More
Opioid Use Disorders Cost U.S. Hospitals More than $95B Annually
What You Should Know:
- Based on prevalence estimates from PINC AI™ data during 2017-2022, an estimated 66 million emergency department (ED) outpatient visits and 760,000 inpatient admissions in the U.S. annually are for patients with the diagnosis of opioid use disorders (OUDs).
- Patients with an OUD diagnosis had 32.5 percent higher cost per ED visit and 8 percent higher cost per inpatient visit than those without an OUD diagnosis. The annual total cost of care for OUD-associated ED
Read More