What You Should Know:
– Prior authorization is mandated by payers to ensure that certain clinical procedures and medications being ordered are necessary. To alleviate the heavy administrative burden this requirement causes, healthcare organizations have adopted automated prior authorization solutions.
– For this report, KLAS interviewed 30 respondents from 26 unique organizations to understand their experiences using these solutions and what outcomes they have seen.
Understanding the Impact Automated Prior Authorization Solutions Provide
This report is a perception study designed to help readers understand where the automated prior authorization market is and what outcomes organizations using automated prior authorization are seeing. To gather these perspectives, KLAS spoke to 30 healthcare leaders from the business office and ambulatory practice administration areas within 26 unique organizations. Interviews were conducted from December 2021 to October 2022.
Here are the key findings:
Automated Prior Authorization Improves Financial Performance and Staff Efficiency
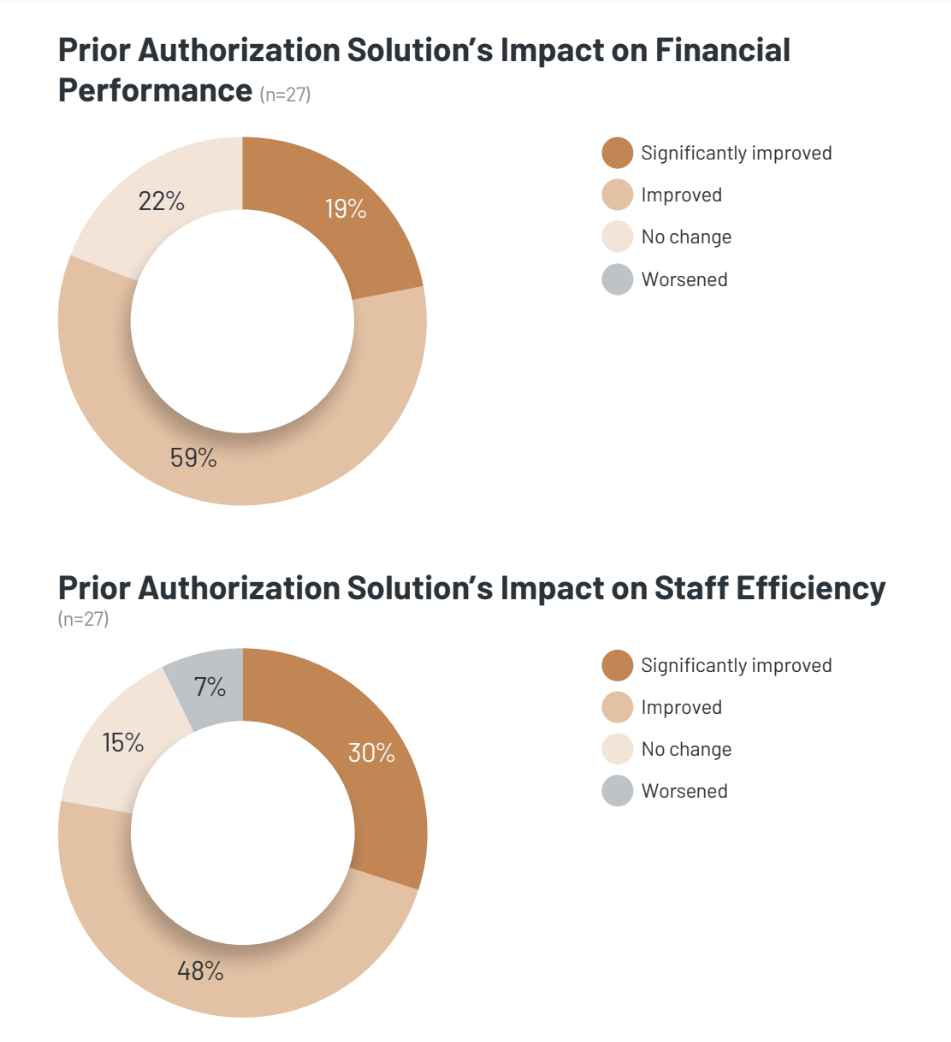
Nearly all interviewed organizations have seen improved financial outcomes and/or staff efficiency from using automated prior authorization. For the 78% of respondents who report improved financial performance, key outcomes include a more efficient, streamlined authorization process; decreased time to approval (within 24 hours), and fewer denials being sent back to provider organizations. While no respondents feel their financial performance has worsened, the remaining 22% have seen no impact and have not achieved outcomes, citing authorizations being returned, not all cases being processed, and the vendor and payer failing to work together to get authorizations approved. Some respondents have also not seen financial outcomes because they haven’t fully implemented their product, preventing them from reaping the full benefits. Increased staff efficiency and reduced staffing needs are also major benefits of automated prior authorization, reported by 78% of interviewed customers. Respondents say streamlined workflows allow them to process more authorizations with the same number of FTEs or to reduce the staffing burden for prior authorization, thus improving ROI. A couple of respondents feel staff efficiency has worsened; they cite poor implementations and the time it takes to get the system up and running.
Expansive Use of Automated Prior Authorization Leads to Higher Satisfaction
Over half of the interviewed provider organizations are using their prior authorization solution for more than 10 payers; of these organizations, two-thirds report their solution works with more than 75% of their associated payers. This expansive use has led to these organizations (which tend to be larger in size) having a higher degree of satisfaction compared to those using their solution for 10 or fewer payers. Respondents who use their solution for more than 10 payers are more likely to be satisfied with the ease of use and highlight simplified, streamlined workflows and the ability to process authorizations without hiring additional FTEs. Most in this group would buy their solution again; in contrast, only 50% of respondents using their solution for 10 or fewer payers would do the same. While prior authorization solutions can work with a large portion of provider organizations’ payers, most respondents note their solution does not yet work with all their payers and hope to see a continued increase in the number of payers their vendors work with.
Customers Want Further Streamlined Workflows, Are Hopeful for Future Improvement
Interviewed customers—even those highly satisfied with their solution— report automated prior authorization could be improved. Some feel their product is clunky and difficult to use; workflows can be hard to set up and cause issues if done incorrectly, and customers want more streamlined workflows to help them achieve more tangible benefits. Implementation times are longer than expected for many organizations, who cite having to go through a challenging process before seeing any benefits. Others note that integration issues (particularly with EMRs) can complicate the implementation process. Customers would benefit from their vendor setting clearer expectations upfront about the difficulties associated with moving to a prior authorization solution. No product’s functionality meets all customers’ needs; across the board, the lowest-scoring metrics for prior authorization solutions are product related. However, many respondents believe in the technology and feel their vendor is moving in the right direction. Some interviewed organizations are expanding or planning to expand their product usage and hope this will improve product performance. Provider organizations appreciate that their vendor can work closely with payers to gather and share the medical criteria necessary for submitting authorizations and also to stay updated on continually changing requirements. Provider organizations that struggle to access medical criteria cite payers’ unwillingness to work with their vendor to provide the necessary information or the vendor’s internal lack of knowledge about guidelines.
Some Friction between Prior Authorization Vendors & Payers; Most Provider Organizations See No Change in Their Payer Relationships from Prior Authorization Solutions
Regarding payer-provider relationships, some interviewed organizations mention that payers can be frustrated with prior authorization vendors due to large automated-transmission volumes or be resistant to provider organizations using prior authorization solutions. Some payers even block vendors’ solutions from accessing necessary information. Despite this frustration, 85% of respondents feel their payer relationships have remained the same and say the friction is largely between vendors and payers. 15% of respondents even report that using automated prior authorization has improved their payer relationships. A few worry about potential issues resulting from the vendor-payer conflict—if a payer chooses to no longer work with a particular prior authorization vendor, the organization then loses access to that payer, undermining the difficult implementation process the organization went through for the prior authorization solution.
“When we were starting with the product, we were sensitive about the impact it would have on our relationship with our payers. But I haven’t seen any big impacts there. I haven’t really felt like there have been any negatives. We have all of these users who are not necessarily bombarding those websites. But I do know that the initial concern was that we were flooding the website with bot interactions rather than user interactions. But I have not heard that that has been an issue from the payer perspective since we have gotten into the system.” —Director
