Anthem Blue Cross and Blue Shield in Maine and MaineHealth today announced the two organizations will be collaborating on a joint venture to offer Medicare Advantage health insurance plans for 2020 under the Anthem | MaineHealth brand. This joint venture effort, named AMH Health, LLC, will bring together the core strengths of the region’s leading health care system and health insurer, their brand recognition, as well as their expertise in providing a comprehensive approach to care that will
Read More
Medicare Advantage | Payers | News, Analysis, Insights
Why Real-Time Health Data Is a Requirement in Today’s Health System
Thanks to technological innovation in the industry and CMS’ push for interoperability, today there’s more patient health data being collected than ever before. The problem is that the data is either not easily accessible to providers or it’s claims based and therefore not timely. The lag time between the collection and sharing of health data makes it difficult, and in some cases impossible, for providers to get a complete picture of their patients’ health, to appropriately treat ongoing
Read More
Medicare Advantage Plans Struggle With Internal Challenges to Keep Pace With Growth
Many Medicare Advantage health plans (35%) struggle with internal challenges in keeping pace with growth, including technology and infrastructure limitations, according to results of its latest Voice of the Market Survey. In addition, 33.8% struggle with a lack of IT staff or resources to make necessary changes and 29.4% lack the in-house Medicare experts necessary to implement adjustments in response to business fluctuation.The survey was commissioned by HealthEdge and conducted by Survata, an
Read More
Innovaccer Launches a Single Data System to Empower Medicare Advantage Plans
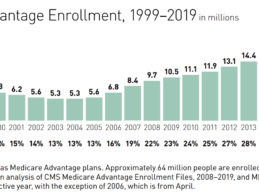
To assist Medicare Advantage plans in eliminating these complications and achieve the top Star Ratings, Innovaccer Inc., a San Francisco-based data activation company, has strengthened its solution for Medicare Advantage plans. The solution for MA plans is a comprehensive suite of solutions designed to solve all grassroots challenges to empower MA plans to ensure healthier patients and increased profits.Rise in Medicare Advantage EnrollmentThe CMS has projected that Medicare Advantage enrollment
Read More
Intermountain Launches Value-based Care Spinout Castell
Intermountain Healthcare has formed a new comprehensive health platform company named Castell that will enable other organizations to accelerate their transition from volume to value-based systems of care, while keeping care more affordable and accessible. Rajesh Shrestha has been named as the president and CEO of Castell. In addition to leading Castell, Shrestha serves as vice president and chief operating officer of Community Based Care for Intermountain Healthcare. He has more than two
Read More
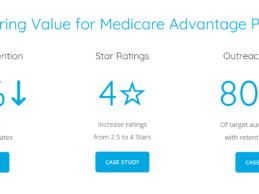
How Medicare Advantage Plans Reduced Their Disenrollment Rates by 30% Through Welltok
The average Medicare Advantage plan turns over about 10% of its members every year, and for a 100,000 member plan, that can equate to about $110 million in lost premium reimbursements as well as a decline in Star ratings. This is why retaining members is a top priority among health plans. Welltok’s Medicare Retention Solution has helped leading Medicare plans reduce disenrollment rates by up to 30%, improve disenrollment-related Star ratings from 2.5 to 4 and retain up to $97 million
Read More
Carenet Health Acquires Engagement, Telehealth Subsidiary of Citra Health
Carenet Health, a San Antonio, TX-based provider of healthcare engagement, clinical support, advocacy and 24/7 telehealth solutions, has acquired the engagement and telehealth solution subsidiary of Citra Health Solutions. The acquisition is the second acquisition of its kind by Carenet in a span of seven months. Financial terms of the acquisition were not disclosed.The recent acquisition complements Carenet’s ongoing commitment to delivering high-quality, cost-effective, on-demand telehealth
Read More
Healthcare’s Uncertain Future: 3 Data-Driven Approaches for Payers
Nine out of 10 healthcare leaders expect disruptive pressures to increase tremendously in the year ahead, according to a recent survey. However, fewer than half believe their organizations are prepared to withstand these forces.
In an era of transformation—in which traditional business models are continually being revamped in response to pressures such as consumerism, policy changes, and the market entrance of non-traditional healthcare players such as Amazon and Apple—payers face daunting
Read More
AdhereHealth And Papa Partner to Tackle Social Determinants of Health
AdhereHealth, a healthcare technology company focused on medication adherence, announced a partnership with Papa, a companionship platform company serving the elderly, blind and disabled. AdhereHealth and Papa will work together to address social determinants of health such as loneliness, food insecurity, and transportation to improve health outcomes for Medicare beneficiaries. The partnership addresses these foundational barriers to care through a combination of advanced technologies and
Read More
3 Ways Health Plans Can Leverage Lab Data Analytics
Payers have long realized the value of leveraging disparate data sets to gain greater insight on patients, with popular data sources including claims, electronic health records, and surveys on social determinants and behavioral health.
More recently, health plans have begun to appreciate another source of data that can help them avoid missed revenues, predict emerging conditions and improve risk management: laboratory data. This category includes data on critical health factors such as
Read More