A glimpse into Meaningful Use Stage 3 considerations and Stage 4 possibilities to understand the overall direction of the future design and use of EHRs.
While most folks are busy trying to keep up with Meaningful Use Stage 1, and Meaningful Use Stage 2 only recently emerged from the customary rulemaking process, those who plan for distant futures are providing us a glimpse of what is being considered for Meaningful Use Stage 3 and here and there a hint at the possibility of a never before mentioned Stage 4 and beyond. Since Stage 2 is still somewhat theoretical, there is little value to enumerating the proposed measures of Stage 3, which is not due to take effect until 2016, but it may prove instructive to take a general look at the overall direction that seems to be favored by policy makers for future design and use of EHR technologies. To that end, several new proposed measures seem most enlightening.
The New US Census Bureau
Stage 1 of Meaningful Use added language, race and ethnicity to the customary demographic information collected from patients, such as name, address, date of birth, gender, etc. Stage 2 proposes to add language, race and ethnicity to clinical summaries provided to patients or sent to other providers of care. So the patient header of a Stage 2 clinical summary might look something like this:

Stage 3 proposes to require the collection of Occupation, Sexual Orientation, Gender Identity and Disability Status in structured, codified format. A futuristic clinical summary header may look a bit more substantial:
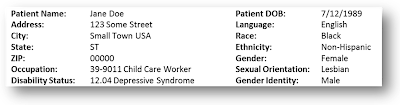
It’s anybody’s guess how long Ms. Doe will be able to keep her minimum wage janitorial job at the little church preschool, once her clinical summary gets circulated among neighborhood providers. The good news of course is that the IOM suggested research agenda on LGBT issues will be significantly advanced, which should eventually benefit Ms. Doe by shading light on disparities she is experiencing a bit more frequently than she expected. With a few more additions to the demographics recording section, perhaps in Stage 5 or 6, we could also save serious federal expenditures on the National Census which should become obsolete following full harmonization with a person’s EHR.
Clinical Decision Surveillance
Meaningful Use Stage 1 began the process of introducing evidence-based advice into clinicians’ workflow and Stage 2 is proposing to broaden availability of helpful alerts and notifications regarding disease management, preventive care and potentially harmful errors. Meaningful Use Stage 3 is contemplating a surge in such activities and is aiming to triple the number of EHR enabled clinical decision “interventions” to 15. To ensure a uniform approach, there seems to be a trend towards externally supplied “interventions”. For example, Stage 4 is mentioning externally maintained drug-drug-interaction (DDI) lists, which is a bit strange since EHRs currently do receive DDI from external sources, such as First Data Bank or Wolters Kluwer anyway, but considering the new ONC sponsored Health eDecisions workgroup and similar other activities, it seems that a centralized approach may be in the works. Thus, Stage 3 is making the initial foray into prescribing clinical decision interventions to include renal dosing checks and “appropriateness” checks for lab and radiology orders. Beginning with Stage 3, it is envisioned that EHRs are able to record and track clinicians’ response to prescribed interventions and in some cases mandates that clinicians view certain information “before” administering immunizations, for example. I think we could save boatloads of money if we required clinicians to install keyloggers on all devices where they might use an EHR from.
On a slightly different note, I find ONCs tortuous grappling with bringing formulary advice from the Pharmacy Benefits Management (PBM) industry into the EHR workflow, somewhat perplexing, since every Surescripts certified electronic prescribing module is already ensuring that PBMs formularies are clearly marked and physicians cannot prescribe anything off formulary without first staring at a screen detailing the PBM’s formulary alternatives (retail, mail-order, copays, etc.), and moreover, the PBMs (who own Surescripts) reserve the right (and exercise it religiously) to approve the actual screen designs for the entire prescribing flow. There is no need to pretend that the Surescripts monopoly doesn’t exist. If ONC needs to make the PBMs happy, Meaningful Use EHR certification should require Surescripts certification, just like CCHIT did in the past.
Bad EHR Design
Meaningful Use Stage 1 logically started with a requirement for EHRs to maintain problems and medications lists. These basic data points have been rolled up into a Clinical Summary requirement in Stage 2, but Stage 3 is proposing advanced ways to improve the accuracy of these lists which are at the heart of a medical record. In Stage 3 EHRs are supposed to be reviewing test results and prescription lists and suggest to physicians additions/edits to the problem list, and in parallel check the current problem list and come up with advice regarding changes to the medication list. The examples given in the Stage 3 document are for the EHR to suggest a diabetes diagnosis if it finds hypoglycemic meds, or to express concerns if it finds an antibiotic lingering around without some appropriate diagnosis. This sounds like the beginnings of magical artificial intelligence, IBM Watson style, because you can only imagine how many diagnoses the EHR could suggest for a particular med or lab test. But then, one question comes to mind: what are these meds and tests without a diagnosis doing there in the first place?
[See also: Meaningful Use Was NEVER About Incenting Physicians To Use EMRs]
A good EHR should not allow anyone to order a test or prescribe a medication without associating it with a diagnosis even if it’s just differential, rule-out, etc. Besides, you need this association if you, or the lab, or the patient, want to get paid for the effort. If we enforce this clinically sound, basic design rule, there should be no need for Watson to weed through garbage data and fix it, and the government should not force such sloppy convoluted design on software products, many of which are already designed correctly. As to finding antibiotics floating around the medication list for no good reason, I wonder if the government is aware that good electronic prescribing systems are either asking for a stop date or are calculating it based on the prescribed quantity (including refills), after which the medication is removed from the active med list. So why should a conscientious EHR designer be forced to implement extremely expensive and fraught with ambiguity algorithms to clean up something that should be clean and buttoned up from the get go? Wouldn’t it be much simpler, more logical and infinitely cheaper to require that all CPOE orders have a diagnosis associated with them when originally entered into the system? And either way, wouldn’t it be wiser to let software builders and their clients make these micro-design decisions on their own?
[See also: CPOE is the Cornerstone of Meaningful Use]
The Road to Hell
One of the most wasteful and aggravating activities in a medical practice is obtaining prior authorizations for various orders. In a valiant effort to come to the rescue, Meaningful Use Stage 4 and beyond is proposing to automate the process, by having physicians enter the necessary information in the EHR and through “web services” automatically receive “real time” authorization (or denial) from payers. Sounds pretty straightforward, but someone should notify the payers. Prior authorization requirements are put in place by insurers to discourage ordering of expensive items, and to that end the process is made so onerous as to make physicians think multiple times before attempting to order something that is not automatically covered. If you look at something as simple as Medicaid drug formularies, there are 50 different sets of rules, one for each State, and then as many more as there are managed care plans in each State, and the rules are different for various medications. Some require stepping through a complex phone triage protocol and are dependent on covered diagnoses (Oregon), some have a special form for each drug, and others have generic forms for all brand names, except a subset of specific brand names. Some specify exactly what supporting documentation is required, while others have nebulous “medical records” requirements. Some have requirements that patients actually suffered an adverse event from stepping through cheap drugs, and in an extremely patient-centered manner are specifying that “client said” or “client reports” is unacceptable (Utah). So much for patient engagement….
To incorporate automated prior authorization into a nationally marketed EHR in a meaningful way, the software would have to computerize thousands of perpetually changing perverse decision trees, with no assurance that the payers will reciprocate the effort. You can make an educated guess regarding the increase in EHR complexity, brittleness and consequently price tags. Wouldn’t it be better for CMS to first standardize the rules for prior authorization across payers, or at least across itself (Medicare/Medicaid and all commercial derivatives thereof)?
[See also: Does Meaningful Use Have Any Unessential Big Feathers to Remove?]
Suggestion
The notion that EHRs and health information technology can be used as a “lever” to alter the business of health care delivery is basically flawed. To date, the only business changes occurring in the health care delivery system are the demise of small private practice and the transformation of health systems into increasingly monopolistic entities, and while the Meaningful Use complexity and expense is not the main driver, it is certainly playing a non-negligible part in this development. Besides, health care delivery is largely dictated by health care financing models, and while I appreciate the difficulty of imposing anything on an industry that spends billions of dollars on lobbying, perhaps CMS can lead by example.
Would CMS consider making its databases available to EHRs through “web services” to obtain demographic and clinical information in “real time” on all Medicare and Medicaid patients? Maybe we won’t be able to get the patient’s BMI or Sexual Orientation, but we should be able to get a pretty accurate (and medical necessity validated) list of problems, medications, procedures, hospitalizations and whatever else CMS paid for, along with the most accurate demographic data (inaccurate claims are denied). Wouldn’t that be a perfect first step in “information exchange”, for the sickest and most expensive patients? And if technology is then shown to cut costs for CMS, wouldn’t private payers follow suit at short notice? Every EHR vendor I know will be fighting to be the first to connect its clients to this data. Perhaps it’s time to impose some meaningful technology and openness rules on the payer side of the house. All the query-response standards for exchanging a minimal, yet extremely valuable, dataset are in place, and all Meaningful Use certified EHRs should be able to process this dataset. How about downsizing and elevating Meaningful Use Stage 3 out of the weeds and branching out to Meaningful Access Stage 1 in 2016?
Margalit blogs regularly about healthcare technology on her site: On Health Care Technology where this article was first posted.
Featured image credit: http://policymed.typepad.com
