Meaningful Use was NEVER about incenting physicians to use EMRs or EHRs. Meaningful Use is about using HIT to improve clinical quality and outcomes.
Level Set
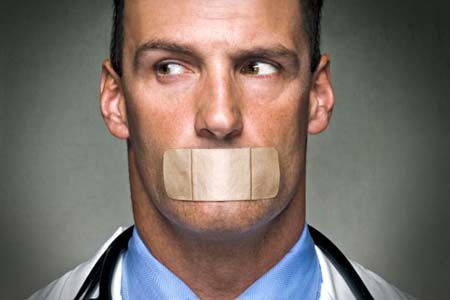
As you know, Meaningful Use has been out there for a little while now, and many have an established impression regarding the primary purpose of the program. I believe that the impression many have about Meaningful Use is inaccurate, and I would like to do a reset before we go any further. The EMR/EHR vendors have been so good at spin that many believe Meaningful Use is really about EMR/EHR adoption. Wrong!
Meaningful Use is not and never was about incenting physicians to use Electronic Medical Records (EMRs) or Electronic Health Records (EHRs). Meaningful Use is about using Health Information Technology (HIT) to improve clinical quality and outcomes. This was a clear directive by CMS when the Stage I Meaningful Use requirements were released, and this priority remains the core purpose for the Stage II requirements as well.
Just the Facts
Let’s take a look at the Stage I Meaningful Use requirements, as described by CMS itself in 2010:
Meaningful Use is using certified EHR technology to improve quality, safety, efficiency, and reduce health disparities.
- Engage patients and families in their healthcare
- Improve care coordination
- Improve population and public health
- All the while maintaining privacy and security
Stage II Meaningful Use takes the ball further downfield with new requirements such as:
- Use clinical decision support to improve performance on high-priority health conditions
- Use clinically relevant information to identify patients who should receive reminders for preventive/follow-up care
- Generate lists of patients by specific conditions to use for quality improvement, reduction of disparities, research, or outreach
- Use Certified EHR Technology to identify patient-specific education resources and provide those resources to the patient
- The EP who transitions their patient to another setting of care or provider of care or refers their patient to another provider of care should provide summary care record for each transition of care or referral.
CMS is more interested in what you DO with your Meaningful Use technology than it is concerned with what TYPE of technology you use to meet the requirements.
Meaningful Use Deconstructed
The Meaningful Use requirements speak to a lot more than using an EMR or an EHR as an electronic file drawer and practicing medicine with your head down – one patient at a time. They speak to goals, processes, and outcomes. They speak to practice transformation. They speak to many of the six pillars of Responsible Population Health Management, which is all about improving outcomes:
| Pillar | Component |
| Point of care tools | Decision support, patient education, patient engagement |
| Care gap analysis | Identifying patients with gaps in their care |
| Patient outreach | Contacting patients to close their care gaps |
| Outcomes reporting | Data analytics and reporting on physician performance |
| Predictive modeling and risk assessment | Identifying high risk patients and analyzing risk at the patient and population levels |
| Care management and coordination | Case management, transitions of care, coordination of care, referral management |
You don’t need to use a traditional EMR or EHR to participate with Meaningful Use. It is common knowledge that many physicians are reluctant to adopt such technologies, which can negatively impact work flow and productivity, are costly to implement and maintain, and were not primarily designed for improving clinical outcomes. CMS knows this. Using a Meaningful Use-Certified Population Health Management system provides an attractive alternative to an EMR/EHR, and such a system can better address your other clinical quality programs, especially at the physician organization or network level.
While this is all true, it’s also not really the primary point of this post. Again, Meaningful Use isn’t about technology, it’s about outcomes.
Intelligent Design
By design, Meaningful Use has been woven into the fabric of other CQI programs and Responsible Population Health Management, and this tapestry includes the many other programs I’ve covered in this series and elsewhere, such as P4P, PCMH, PQRS, and Accountable Care. The work you do for any one of these programs carries over to each of the other programs.
So, don’t think of Meaningful Use as a separate program or topic, rather think of it as yet another program that helps you establish and organize your organizational goals, processes, and desired outcomes. Don’t put the Meaningful Use payment of $44,000 – $63,750 per provider in a separate bucket, rather put it in the same category as the incentive payments you may receive from P4P, PCMH, PQRS, Accountable Care, and any other clinical quality improvement initiatives in your region. They are all related.
At the end of the day, technology merely enables you to improve clinical quality outcomes; it doesn’t do the work for you. In order to improve outcomes and reduce the cost of health care, physicians and their organizations need to be proactively engaged in the process.
Meaningful Use is tightly linked to other commonly encountered CQI programs and provides a solid framework and respectable incentives, so make sure this tool is in YOUR physician engagement shed.
Dr. Taylor is the co-founder of Wellcentive and blogs regularly about physician engagement where this was first posted.