Rising operating costs, shrinking operating margins, and a complex payer landscape characterized by heightened prior authorization requirements and a push to embed advanced technology more deeply into the review process have thrown provider finances into turmoil. Exacerbating it all is a chronic and worsening shortage of skilled revenue cycle management (RCM) professionals, including patient access.
Internally, the inefficiencies created by outdated, time-consuming, and
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
Rectangle Health& ECHO Health Partner to Automate Claims Payments
What You Should Know:
- Rectangle Health, a recognized leader in healthcare technology solutions, today announced a partnership with ECHO Health, Inc. (ECHO®), a payments company focused on removing complexity, costs, and fraud risk from payment processing.
- This collaboration grants healthcare organizations unprecedented access to automated claims payment processing, Explanations of Payments (EOPs), and posting via the industry’s most comprehensive digital payment
Read More
Frazier Healthcare Partners Sells Elevate Patient Financial Solutions to Audax and Parthenon
What You Should Know:
- Frazier Healthcare Partners (“Frazier”), a private equity firm focused exclusively on the healthcare sector announced the sale of Elevate Patient Financial Solutions (“Elevate” or the “Company”) to Audax Private Equity and Parthenon Capital. Financial terms of the transaction were not disclosed.
- Elevate, headquartered in Spring, TX, is a leading provider of technology-enabled specialty revenue cycle management (“RCM”) services for hospitals and health systems,
Read More
Ledger Lines to Neural Nets: Re-engineering Medical Coding for the GPU Age
In 1971, a small team at Boston’s Beth Israel Hospital, led by Dr. Howard Bleich and Dr. Warner Slack, booted up the hospital’s first Center for Clinical Computing. Their PDP-11 minicomputer stored lab results and a few hundred ICD-8 codes on nine-track tape. Each evening, residents lined up to run charge‐slip reports and marvel at the glow of the terminal. Fifty years later, we still tabulate charges, but the code set has grown from those few hundred entries to nearly 70,000 in ICD-10-CM,
Read More
Waystar to Acquire Iodine Software for $1.25B, Enhancing AI-Powered Healthcare Payment Solutions
What You Should Know:
- Waystar, a provider of healthcare payment software announced a definitive agreement to acquire 100% of Iodine Software (“Iodine”) for $1.25B.
- The proposed acquisition is expected to significantly accelerate Waystar’s ability to transform healthcare payments through its leading cloud-based software platform, empowering more than one million providers with advanced AI capabilities to prevent denials, reduce manual work, and improve financial
Read More
UnitedHealth Group Under DOJ Probe: Medicare Billing Practices Face Criminal & Civil Investigation
What You Should Know:
- UnitedHealth Group revealed it is facing a Justice Department (DOJ) criminal and civil investigation into its Medicare billing practices, adding to a series of recent setbacks for the nation’s largest and most powerful private insurer.
- The company also announced it has launched a third-party review of its business policies and performance metrics, expected to be completed by the end of the third quarter. The announcement comes after a tumultuous period for
Read More
Humana Accelerates Prior Authorization Reforms, Pledges to Cut Requirements and Expedite Approvals
What You Should Know:
- Humana Inc. announced accelerated efforts to approve care requests as quickly as possible and reduce the administrative burden for physicians associated with prior authorization.
- These actions aim to streamline and reduce prior authorization requirements while preserving the system of checks and balances that protects patient safety for high-cost, high-risk treatments.
Prior Authorization Reform
Humana is working to reduce the "red tape" on prior
Read More
TechMatter Acquires DoctorPapers to Expand Healthcare Revenue Cycle Management Services
What You Should Know:
- TechMatter, a leading provider of enterprise healthcare and automation solutions, acquires DoctorPapers, a California-based medical billing and revenue cycle management (RCM) company. This strategic move reinforces TechMatter’s mission to deliver scalable, tech-driven healthcare operations to providers across the United States. Financial details of the acquisition were not disclosed.
- Founded in 2020, DoctorPapers has built a strong reputation for delivering
Read More
Charta Health Secures $22M to Automate Medical Billing and Clinical Documentation with AI
What You Should Know:
- Charta Health, an AI-powered platform that automates and optimizes medical billing and clinical documentation workflows secures $22M in Series A funding round led by Bain Capital Ventures, with participation from Madrona, SV Angel, Refract Ventures, and South Park Commons.
- The U.S. healthcare system loses over $300 billion each year due to billing errors, undercoding, and preventable claim denials. This significant financial drain often stems from slow,
Read More
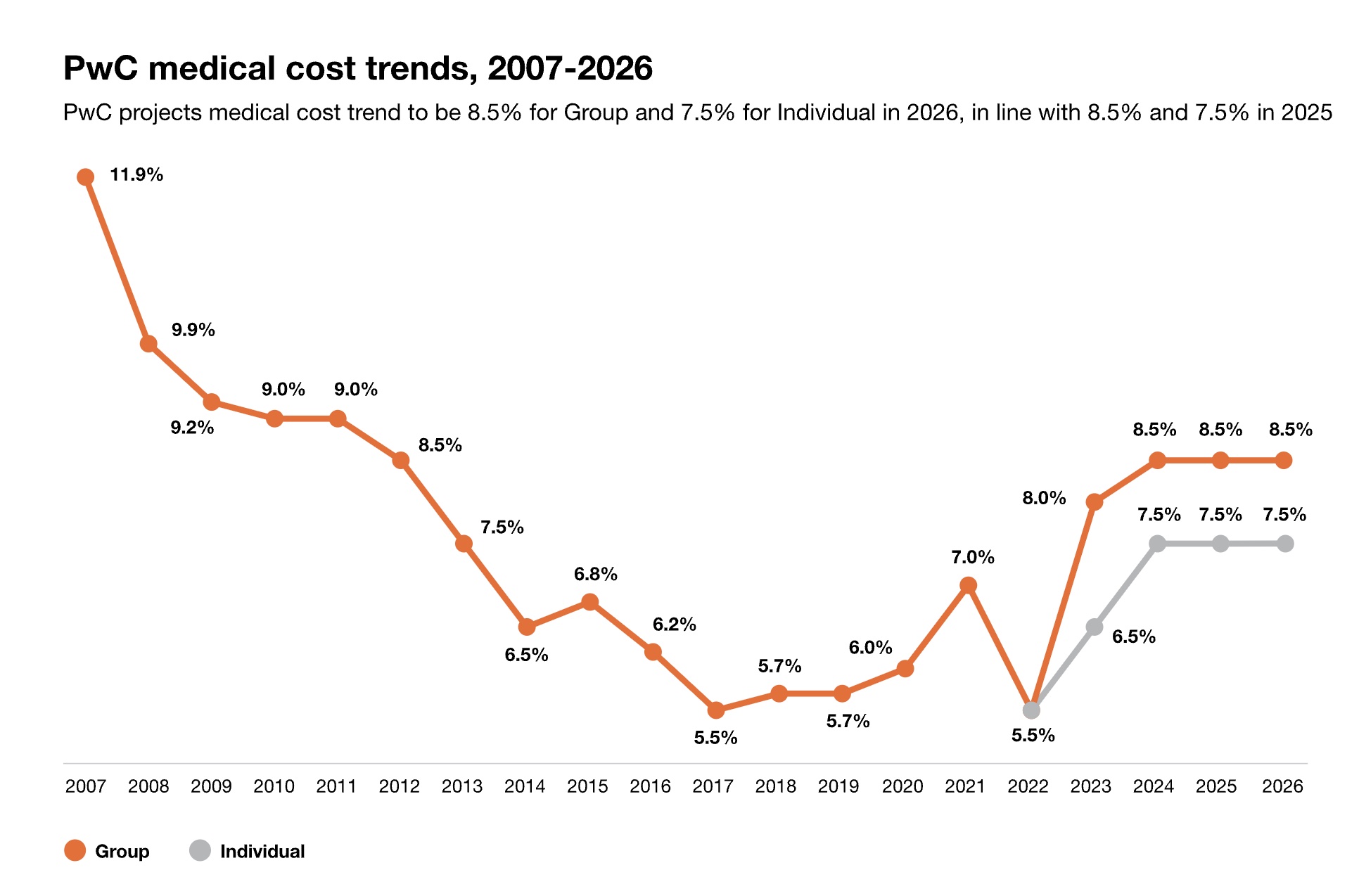
PwC Report: US Medical Cost Trend to Remain Elevated at 8.5% in 2026
What You Should Know:
- The U.S. healthcare system is entering 2026 with medical cost trends reminiscent of 15 years ago, facing persistent inflationary forces and significant federal policy changes, according to a new report from PwC.
- The report, "Medical Cost Trend: Behind the Numbers 2026," projects the Group medical cost trend to remain at 8.5% in 2026 (the same level as 2025) and the Individual market trend at 7.5%. Pharmacy costs are a particular concern, projected 2.5
Read More