The Crisis Facing Healthcare Financial Leaders
Healthcare financial leaders are navigating an environment of unprecedented complexity. Your organization is caught between escalating operational costs and a relentless denial rate fueled by increasingly sophisticated payer tactics. The truth is, if your Revenue Cycle Management (RCM) is reliant on manual, legacy systems, you are accepting a permanent, self-inflicted fiscal vulnerability.
Industry data confirms this exposure: upwards of 10%
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
Denial Management: Closing Gaps and Reducing Revenue Leakage
Revenue leakage on the front end and mid-cycle is an ongoing challenge for hospitals and health systems. Rather than taking a reactive approach to the problem, proactively collaborating among teams prior to admission helps providers avoid playing the blame game when their claims are denied after the fact.
By focusing on reducing the number of denials before a claim is submitted, rather than trying to eliminate denials after the fact, revenue cycle managers can save time and energy. Today’s AI
Read More
From Confusion to Collections: How Unclear Billing Fuels the Medical Debt Crisis
Medical debt remains a significant burden for patients nationwide, with U.S. residents collectively owing an estimated $220 billion. Medical visits already bring emotional and financial stress, and confusing bills only make matters worse. When patients receive statements that they don’t understand, or multiple, fragmented bills, they’re left frustrated, less likely to pay on time, and are at greater risk of accumulating medical debt.
While the July 2025 ruling striking down the Consumer
Read More
Beyond the Margin Squeeze: How Specialty Providers Use RCM Automation to Combat Rising Costs
Despite a recent uptick in margins, providers continue to face significant pressure on their revenue cycles as a result of potential reimbursement cuts, workforce recruitment challenges, and higher costs.
Providers in 2024 reported operating margins of 1.2%, up from -0.5% the prior year, according to a report from Fitch. Nonetheless, margins remain “well below” pre-pandemic levels, and looming federal cuts to Medicaid funding could be devastating for some providers.
Federal
Read More
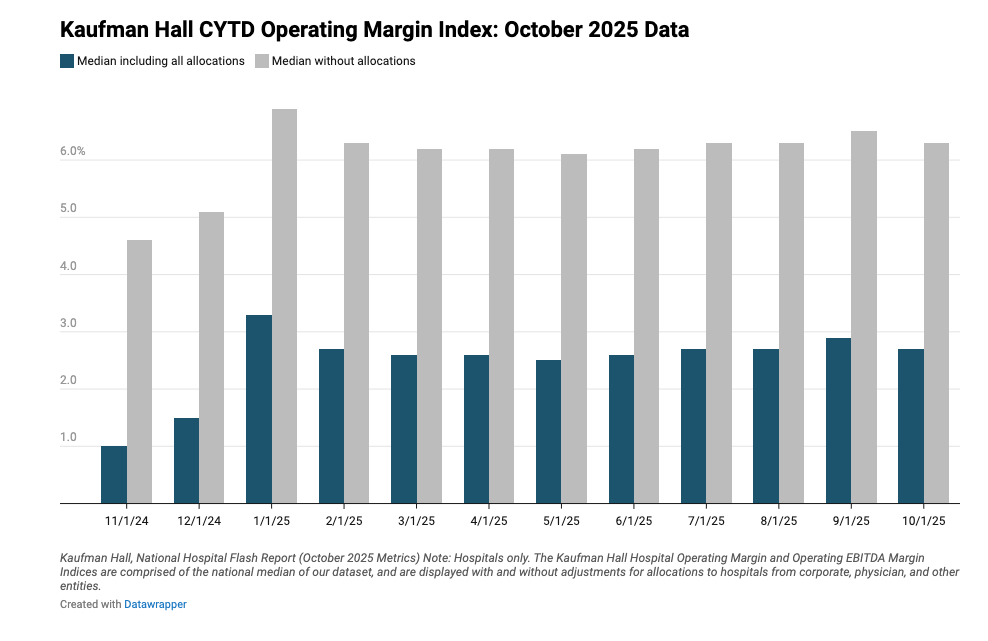
Kaufman Hall Report: Rising Non-Labor Costs and Payer Denials Squeeze Hospital Margins in 2025
What You Should Know:
- According to Kaufman Hall’s 2025 Health System Performance Outlook, hospitals are facing a "financial trifecta" of rising non-labor expenses, workforce instability, and aggressive payer reimbursement pressures.
- Nearly 60% of health systems reported non-labor cost increases of up to 10%, driven by inflation and tariffs, while 44% cited high claim denial rates as a top challenge. As bad debt rises and staffing levels tighten, the report urges leaders to
Read More
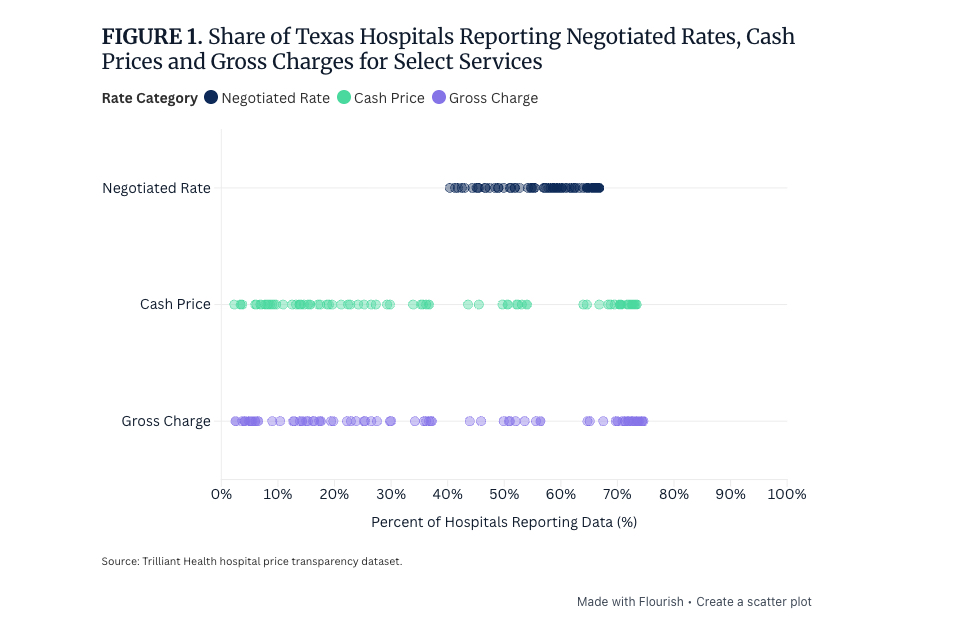
Transparency Trap: Why Commercial Negotiated Hospital Rates Are Up to 32% Higher Than Cash Prices
What You Should Know:
- New analysis of Texas hospital price data reveals a transparency paradox: discounted cash prices for common services are often significantly lower than the rates hospitals negotiated with commercial insurers, according to a new research study from Trilliant Health.
- For diagnostic colonoscopies, the median cash price was 32% below the median negotiated rate. This disconnect means that employees on high-deductible health plans (HDHPs) and the employers who
Read More
Commure Autonomous Coding Scales to 200+ Sites with OBHG: Clinicians Reduce Charge Time by 83%
What You Should Know:
- Commure, a healthcare technology company, and Ob Hospitalist Group (OBHG), the nation's largest provider of OB/GYNs, have formed a strategic partnership to deploy Commure’s Autonomous Coding solution across nearly 2,000 clinicians and over 200 care sites.
- Early results are compelling: within three months, clinicians reduced the time spent entering charges by an impressive 83%, with AI now coding over 85% of all charges. This deployment strengthens
Read More
Why Faster Prior Authorizations Won’t Fix Healthcare’s Real Issues
Few phrases raise blood pressure among doctors and patients like “prior authorization.” Ask any clinician and you’ll hear the same story: delayed treatments, endless back-and-forth, and vulnerable individuals left waiting while paperwork wins the day.
For providers, prior authorizations are a constant drain of time and energy. For patients, they can mean worsening conditions, missed windows for effective treatment, or even care that never arrives at all. And for payers, prior
Read More
AdvancedCare Launches Inbox Health Partnership for 350 Behavioral Health Clinics
What You Should Know:
- Inbox Health, a patient billing and engagement technology platform, today announced a strategic partnership with AdvancedCare, an AI-driven practice management, EMR, and revenue cycle solution.
- The collaboration integrates Inbox Health’s automated billing communication and payment technology with AdvancedCare’s AI Clinical and Revenue Cycle Management (RCM) platform. This unified solution directly targets behavioral health and psychiatry clinics, segments often
Read More
Denial Prevention AI: Ember Raises $4.3M to Cut Healthcare Denials by Over 57%
What You Should Know:
- Ember, the AI-native solution for denial prevention secures $4.3M in seed funding round led by Nexus Venture Partners and Y Combinator.
- Its platform uses deep knowledge of payer policies to cut denials by more than 57% and boost net collections by 25% for health systems.
The Denial Crisis: Fueling Burnout and Financial Loss
Healthcare providers nationwide face an intensifying crisis driven by claim delays and denials, which create significant
Read More