What You Should Know:
- Healthcare industry leaders Ventra Health and ADVOCATE RCM announced a groundbreaking merger today, joining forces to become one of the nation's largest and most advanced providers of end-to-end revenue cycle management (RCM) services.
- This strategic move expands Ventra's reach beyond its core specialties in anesthesia, emergency medicine, and hospital medicine, while ADVOCATE RCM gains access to Ventra's extensive resources and network.
Merger Impact
Ventra
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
M&A: Veradigm Acquires Koha Health to Strengthen Ambulatory RCM
What You Should Know:
- Veradigm Inc. (NASDAQ: MDRX), a leading healthcare data and technology solutions provider, announced today the acquisition of Koha Health, a full-service revenue cycle management (RCM) company.
- This strategic move strengthens Veradigm's position as a premier provider of RCM services in the ambulatory healthcare market. Financial details of the acquisition were not dislcosed.
Expanding Ambulatory RCM Expertise and Reach
The acquisition brings
Read More
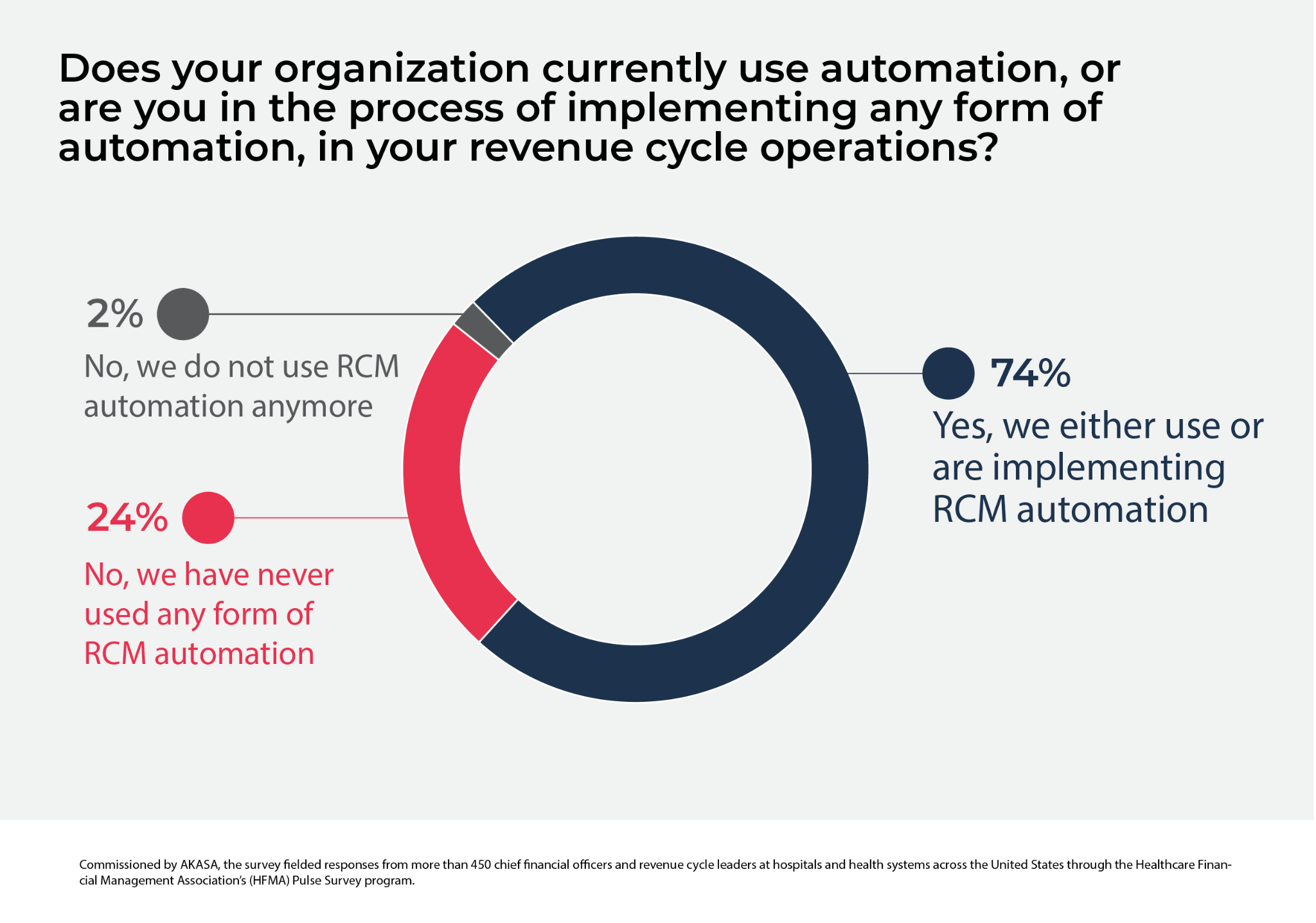
RPA Adoption: 74% of Hospitals Automate Revenue Cycle Tasks
What You Should Know:
The healthcare revenue cycle is getting a major makeover, driven by a surge in automation and artificial intelligence (AI). A new survey by AKASA, a leading developer of AI-powered revenue cycle automation solutions, reveals that 74% of healthcare organizations are already automating some part of their revenue cycle operations, and 80% of those not currently using it plan to do so by the end of 2025.
The Rise of the Robots
- Automation is no longer a luxury, but a
Read More
KAID Health Secures $9M to Drive AI-Driven Healthcare Efficiency
What You Should Know:
- KAID Health, the AI-powered healthcare solutions pioneer, has secured a significant $9 million in funding led by Activate Venture Partners, Martinson Ventures, Boston Millennia Partners, and Brandon Hull, alongside KAID Health's Board of Directors.
- With this new funding, KAID Health plans to expand its reach to more providers and their payer partners and develop new service offerings.
Unlocking the Power of Whole Chart Analysis
KAID Health's flagship
Read More
TREND Health Acquires Advent for AI-Powered Healthcare Payment Accuracy
What You Should Know:
- TREND Health Partners, a rapidly growing provider of AI-driven solutions, has acquired Advent Health Partners, an AI-driven platform identifies and standardizes clinical attributes from itemized bills and medical records, expediting critical information presentation and ensuring timely and appropriate reimbursement.
- This strategic combination brings together two industry powerhouses, creating a comprehensive platform for payers and providers seeking to optimize
Read More
Rise of RCM Managed Services: 95% of Healthcare Execs Embrace RCM Outsourcing
What You Should Know:
- Ensemble Health Partners, a provider of revenue cycle management services, has released its 2024 Healthcare Business Trends Report, revealing a shift in priorities among healthcare executives.
- The report, based on a survey of over 100 senior executives, highlights a growing focus on outsourcing revenue cycle management and leveraging external expertise to drive performance, improve financial health, and achieve long-term growth.
4 Trends Driving the Next 4
Read More
R1 RCM Acquires Acclara for $675M, Secures 10-Year RCM Partnership with Providence Health System
What You Should Know:
- R1 RCM Inc. (NASDAQ: RCM), a provider of technology-driven solutions for healthcare providers, announced a significant strategic partnership involving the acquisition of Acclara and a 10-year revenue cycle management agreement with Providence, one of the nation's largest health systems.
- The acquisition of Acclara for $675M in cash and warrants will bolster R1's offerings and position it as the "trusted partner of choice" in comprehensive revenue cycle management.
Read More
4 Ways AI Is Enhancing The Patient Experience in 2024
Artificial intelligence (AI) captured the imagination of many in 2023. AI gets a lot of attention but little understanding or appreciation of what it can do to move revenue cycle management (RCM) forward, improve the patient experience, and answer the question, “Are you receiving the appropriate reimbursement?”
More than 3 of 5 companies are still experimenting with AI, according to a recent survey by Accenture. Only one in four are innovating or achieving stated objectives) and
Read More
HFMA and FinThrive Launch Revenue Cycle Management Technology Adoption Model
What You Should Know:
- The Healthcare Financial Management Association (HFMA) has announced a strategic alliance with FinThrive, Inc., a healthcare revenue cycle management (RCM) software-as-a-service (SaaS) provider, to co-launch a peer-reviewed, five-stage Revenue Cycle Management Technology Adoption Model (RCMTAM).
- The RCMTAM is designed to help health systems leverage industry benchmarks to assess their current state of RCM technology maturity and build best-practice plans to
Read More
M&A: Experian Acquires Wave HDC to Enhance Healthcare Coverage Identification and Automation
What You Should Know:
- Experian acquires Wave HDC, a healthcare technology leader that offers AI-enhanced data curation solutions to identify unknown insurance benefits coverage and critical patient demographics at the start of a patient's healthcare journey.
- The acquisition bolsters the Experian Health business portfolio with more comprehensive and faster healthcare coverage identification and automation capabilities.
Wave HDC's AI-Powered Solutions
Wave HDC offers several
Read More