What You Should Know
The Reality: The U.S. healthcare system is in a "structural pressure" cooker. While patient outcomes are improving (mortality down 33%), the financial model is fracturing under the weight of an aging population and rising supply costs.The Shift: 2026 marks the end of the "Megadeal" era. Hospital M&A has pivoted to distressed asset acquisitions, while successful systems are moving toward vertical partnerships rather than buying more hospitals.The Future: AI is the only
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
Ventra Health Launches “vCision” – An Agentic AI Platform to Combat Revenue Leakage
What You Should Know
The News: Ventra Health has launched vCision, a new revenue intelligence platform powered by "Agentic AI" (autonomous digital agents) to optimize the revenue cycle for facility-based physicians.The Partnership: The platform was developed in partnership with healthcare engineering firm CitiusTech, combining Ventra’s RCM expertise with CitiusTech’s generative AI capabilities.The Goal: vCision aims to move beyond simple automation by using adaptive models to anticipate payer
Read More
Consolidating Clinical Intelligence: Rapid Care Acquires DeepDoc to Scale AI Summarization
What You Should Know
The Deal: Rapid Care has acquired DeepDoc, a generative AI platform specializing in summarizing complex medical records with over 99% accuracy. Financial details of the acquisition were not disclosed. The Problem Solved: The technology addresses the "unstructured data" crisis in healthcare by automating the review of massive patient files for insurance claims, legal cases, and utilization reviews.Acquisition Impact: This is Rapid Care’s third major acquisition in three
Read More
Kaiser Permanente Affiliates to Pay $556M to Settle Medicare Advantage Upcoding Allegations
What You Should Know:
- Kaiser Permanente affiliates have agreed to a $556M settlement to resolve allegations of violating the False Claims Act by submitting invalid diagnosis codes to inflate Medicare Advantage (MA) payments.
- The settlement, involving multiple Kaiser Foundation and Permanente Medical Groups, addresses a decade-long "data mining" scheme designed to pad the bottom line by manipulating the risk-adjustment model.
The Core of the Conflict: Risk Adjustment vs. Care
Read More
How Hospital M&A Momentum Shifted to Ambulatory and Behavioral Health in 2026
What You Should Know
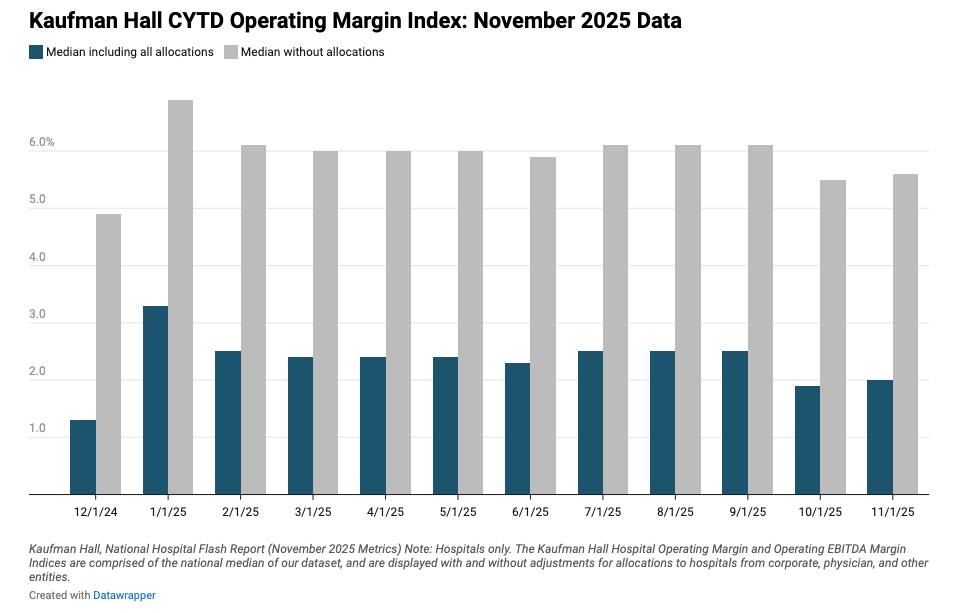
- Kaufman Hall has released its year-end analysis for 2025, reporting a total of 46 hospital and health system transactions. While total transacted revenue hit a historical low of $18.5 billion due to a slow start in the first half of the year, momentum surged in Q4 with 17 transactions, including four "mega mergers" where the smaller party’s annual revenue exceeded $1 billion.
- Crucially, financial distress drove a record 43.5% of all transactions, a trend
Read More
The Autonomous Revenue Cycle: Waystar Launches Agentic AI to Prevent Billions in Denials
What You Should Know
- Healthcare payment provider Waystar has announced the introduction of agentic intelligence to its cloud-native platform, marking a pivotal step toward the industry's first autonomous revenue cycle.
- Powered by the Waystar AltitudeAI™ engine and a dataset comprising 7.5 billion annual transactions, the new agentic network is designed to execute defined tasks and learn from outcomes with minimal intervention, significantly reducing administrative friction for
Read More
HPS/PayMedix Secures $33M to Scale Guaranteed Healthcare Payments
What You Should Know
- HPS/PayMedix secures $33M in combined equity and debt financing to accelerate the growth of its healthcare financing and payments platform.
- Led by HLM Investment Partners, the funding will be used to expand the PayMedix solution, which unifies all healthcare stakeholders through guaranteed provider payments, interest-free patient financing, and a consolidated SuperEOB® experience.
The Affordability Mandate: Unifying the Payment Experience
As
Read More
FinThrive Report Reveals 71% of RCM Leaders Prioritize Experience Over Revenue
What You Should Know
- FinThrive's 2026 Transformative Trends Report marks a historic turning point: for the first time, improving the patient experience has surpassed increasing revenue as the top strategic goal for healthcare financial leaders, with 71% identifying it as their primary focus.
- The shift indicates that leaders are moving away from short-term fixes toward AI-enabled platform consolidation and automation to drive long-term stability and workforce
Read More
Zelis Acquires Rivet to Bring AI-Powered Analytics to 750+ Providers
What You Should Know
- Zelis, a global leader in healthcare financial modernization has acquired Rivet, a pioneer in revenue cycle analytics. Financial details of the acquisition were not disclosed.
- The deal integrates Rivet’s AI-enabled analytics and intuitive dashboards directly into the Zelis platform, providing 750+ payers and millions of providers with actionable data to reduce denials, minimize "rework," and navigate rising regulatory complexity.
The Intelligence Layer:
Read More
Abridge and Availity Partner to Automate Prior Authorization at the Point of Conversation
What You Should Know
- Abridge, the leader in clinical conversational AI, and Availity, the nation’s largest health information network, have launched a first-of-its-kind collaboration to automate prior authorization in real-time.
- By embedding Availity’s FHIR-native Intelligent Utilization Management solution into Abridge’s Contextual Reasoning Engine, the partnership aims to provide clinicians with visibility into coverage requirements and enable payer determinations during the
Read More