What You Should Know:
- SPRY PT today unveiled the industry’s first AI-powered Prior Authorization & Eligibility solution, proven to automate 80% of the prior authorization workflow while ensuring 100% of authorizations are completed through a combination of AI automation and expert review.
- The solution reduces related denials by up to 75%, streamlines workflows across major payers including Carelon/BCBS, UnitedHealthcare, and Humana, and provides unlimited, real-time eligibility
Read More
Automated Prior Authorizations
Inovalon and Google Cloud Partner to Launch AI-Enabled Prior Authorization Solution
What You Should Know:
- Inovalon, a provider of solutions that empower data-driven healthcare, has announced a new collaboration with Google Cloud to develop an AI-enabled solution designed to address administrative burdens in the healthcare industry.
- The partnership will combine Inovalon’s extensive data solutions and subject matter expertise with Google Cloud's advanced AI and machine learning capabilities to tackle time-consuming prior authorization processes.
A Vision for
Read More
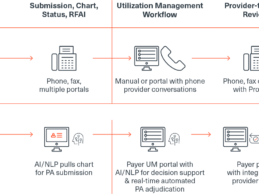
ZeOmega Partners With Datycs to Optimize Prior Authorization
What You Should Know:
-ZeOmega®, the leading population health management organization, today announced its partnership with Datycs, a leading provider of clinical AI/Natural Language Processing (NLP) solutions, to automate converting unstructured data from faxed documents into standardized, interoperable, and actionable information.
- The collaboration will help health plans garner insights that will drive improvements in member care, provider and payer workflows, and overall
Read More
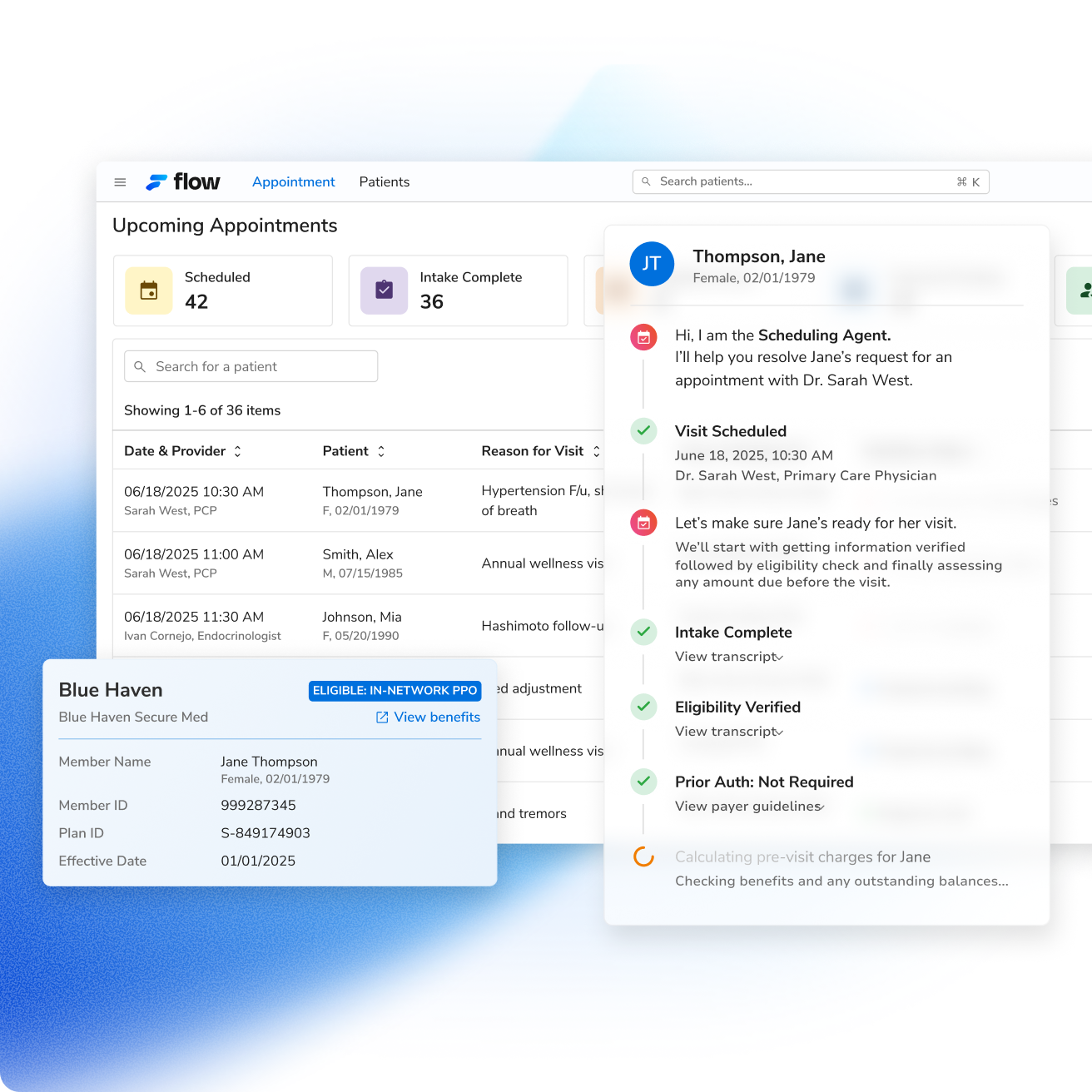
Innovaccer Launches AI-Powered Prior Authorization Solution: Flow Auth
What You Should Know:
- Innovaccer Inc., a healthcare AI company launches Flow Auth, a new AI-powered prior authorization solution.
- As part of the company's revenue cycle performance platform, Flow by Innovaccer, Flow Auth is designed to automate the entire prior authorization (PA) workflow, helping healthcare organizations accelerate care delivery and optimize revenue capture.
- Innovaccer projects that the solution could lead to a 50% reduction in the time clinicians
Read More
RISA Labs Raises $3.5M for AI-Powered Oncology Prior Authorizations Platform
What You Should Know:
- Cancer patients don’t just fight the disease - they fight the system. Today, life-saving treatments are routinely delayed by days or even weeks due to manual, error-prone workflows
- To solve this, RISA Labs has raised a $3.5M funding round to help healthcare organizations eliminate one of the most persistent barriers to timely cancer care: prior authorization delays. RISA Labs has already proven that faster care is possible by dramatically reducing manual
Read More
Evolent Acquires Machinify’s AI-Driven Medical Authorization Solution
- Evolent Health, Inc. (NYSE: EVH), a leader in improving health outcomes for patients with complex conditions, announced today an agreement to acquire key assets from Machinify, including the exclusive license to their AI-powered platform, Machinify Auth.
- Additionally, certain Machinify employees will join Evolent. Both companies plan to establish a long-term services agreement to ensure smooth integration and ongoing platform development. This innovative technology aims to
Read More
Humana Expands Use of Cohere Health’s Prior Authorization Platform
What You Should Know:
- Cohere Health, a recognized leader in clinical intelligence and prior authorization automation, announced that Humana Inc. (NYSE: HUM) will expand its use of Cohere's prior authorization platform for diagnostic imaging and sleep services.
- In January 2021, Cohere and Humana began a pilot
Read More
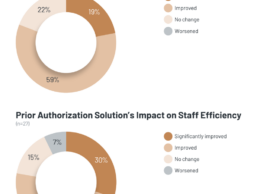
KLAS: What Impact Do Automated Prior Authorization Solutions Provide?
What You Should Know:
- Prior authorization is mandated by payers to ensure that certain clinical procedures and medications being ordered are necessary. To alleviate the heavy administrative burden this requirement causes, healthcare organizations have adopted automated prior authorization solutions.
- For this report, KLAS interviewed 30 respondents from 26 unique organizations to understand their experiences using these solutions and what outcomes they have seen.
Understanding
Read More
HLTH22 Day 3 News Summary
DispatchHealth Raises $330M for Hospital-at-Home Care
DispatchHealth, a provider of in-home medical care raises $330M led by Optum Ventures with support from current investors such as Humana (NYSE: HUM), Oak HC/FT, Echo Health Ventures and Questa Capital. New investors included Adams Street Partners, the Olayan Group, Silicon Valley Bank, Pegasus Tech Ventures and Blue Shield of California. Patients and their care partners can request DispatchHealth medical care via phone, mobile app, or
Read More
Edifecs Partners with Empowered-Home to Deliver Automated Prior Authorizations
What You Should Know:
- Edifecs and Empowered-Home announced a partnership to provide automated prior authorizations to medical associations, Accountable Care Organizations (ACOs), Independent Physician Associations (IPAs), medical groups, and home health care agencies.
- The Edifecs prior authorization solution combined with the clinical decision support system of patient management software company, Privis Health, forms the backbone of Empowered-Home’s ecosystem. Empowered-Home is
Read More