
An introduction to asynchronous, or store-and-forward, as a modality of telehealth
As our healthcare system continues to innovate in order to meet demands and improve the delivery of value, various telehealth solutions have emerged and been implemented to increase efficiency, access to, and quality of care. Telehealth is a broad term encompassing “a collection of technology-based means or methods to enhance healthcare delivery and education.” As defined by the National Telehealth Resource Center, four distinct modalities of care fall under telehealth:
– Live video conferencing (synchronous) Store-and-Forward (asynchronous)
– Remote Patient Monitoring (RPM)
– Mobile Health (mHealth)
Of particular interest is asynchronous telehealth, which is steadily gaining traction in the healthcare field.
Asynchronous telehealth is defined as the transmission of recorded health history through an electronic communications system to a practitioner, usually, a specialist, who uses the information to evaluate the case or render a service outside of real-time or live interaction — thus enabling providers to access specialist input within their own workflow.
The most common form of asynchronous telehealth is eConsults, commonly used in radiology, pathology, dermatology, and ophthalmology. In ophthalmology, for instance, eye screenings for diabetic retinopathy can be captured digitally by retinal cameras and transmitted to a specialist for review. The eConsult segment of telehealth has improved access, quality, satisfaction, and efficiency for many patients by reducing unnecessary referrals and allowing patients to be treated more often.
Despite its usefulness, however, asynchronous telehealth is frequently overlooked by healthcare providers planning and budgeting for a telehealth strategy. This is generally due to a lack of understanding of how this modality fits into an overall telehealth strategy and uncertainties surrounding reimbursement for use of associated technologies. Therefore, it seems prudent to introduce asynchronous telehealth, specifically highlighting its benefits and common forms, as well as outlining how reimbursement changes allow this important option to fit more easily into a truly complete telehealth strategy.
The Benefits of Asynchronous Telehealth Solutions
Healthcare providers who have added asynchronous telehealth technologies to their workflow have seen several clear benefits that improve healthcare delivery for all parties involved. Patients, for instance, enjoy increased efficiency in accessing specialist care, avoiding the long wait times generally associated with making a specialist appointment. This increases the overall quality of care and also avoids complications such as specialists being out of network, and thus prohibitively expensive. Store-and-forward technologies can also help patients overcome language barriers that may cause difficulties with audio-visual technologies.
When it comes to physicians, both PCPs and specialists see benefits from asynchronous telehealth. PCPs can get necessary input regarding their patient while retaining control over care and coordination, versus care that is delivered directly to the patient either virtually or via a specialist appointment. Specialists, meanwhile, can review patient cases when it’s convenient for them. Specialists are also generally able to review more cases via store-and-forward platforms. A doctor with an hour of free time could conceivably handle 20 cases on an asynchronous platform, while they might be able to complete four or five cases on an audio-visual platform. In addition, with the use of live audio-visual platforms, both parties must connect in real-time versus at their own convenience.
Finally, asynchronous platforms allow health system administrators to configure workflows around an existing provider base – letting them include the program in their normal routine or pay out a smaller per-case fee. Further, by nature, all information is reliably documented in writing and can be uploaded as part of the patient’s health record, so providers can return to consultations to review information at any time. This also makes store-and-forward ideal for evidence-based care, as providers are easily able to gather all information on a patient, analyze the data, and make an informed diagnosis.
eConsults as a Key Asynchronous Solution
eConsults, or electronic consultation, is a common form of asynchronous telehealth that has been widely adopted and shown significant improvement in the delivery of care. An eConsult platform connects primary care doctors with on-demand specialists who can review and consult on cases that would be otherwise referred for specialist appointments. eConsults improve access to care by allowing primary care providers to treat a large percentage of routine referrals within primary care, backed by specialist guidance. This, in turn, better triages referrals to reduce appointment wait times for those patients in need of face-to-face appointments and expedites care for those who can be managed within primary care. eConsults have shown to be especially effective in improving access and quality within underserved populations who face significant challenges in accessing the care they need.
eConsults support a closed-loop referral system, where a primary care provider can effectively act to coordinate care and follow-up from direct communication with specialist and patient regarding the treatment plan. In addition, eConsults better prepare patients for a more effective conversion to face-to-face specialty referrals if needed. Workups and necessary diagnostics can be completed within primary care following specialty guidance before appointments. This reduces unnecessary appointments and duplicative testing, as well as time spent waiting for care.
Successful asynchronous telehealth programs have been implemented all over the world.
The Champlain BASE™ eConsult Service in Ontario, Canada, for example, connects primary care providers and specialists. The program has been hugely successful, having secured over 2 million dollars in funding and reaching a level of national collaboration.
Another positive aspect of asynchronous telehealth solutions is the ability to efficiently and seamlessly integrate into clinical workflows. eConsults are now available for integration with Epic through the Epic App Orchard Marketplace. This eConsult integration enables clinicians to launch the telehealth platform directly through the clinic EHR, creating a user-friendly experience for answering eConsults with minimal provider burden and workflow changes.
Reimbursement Available for Asynchronous Telehealth Solutions
Reimbursement has been one of the biggest barriers in terms of adopting telehealth platforms. Recently, however, the Centers for Medicare and Medicaid Services (CMS) has begun to recognize the value of these platforms, reflected by new codes and associated reimbursement for eConsults were finalized in the 2019 CMS Clinical Lab Fee Schedule. These updates expand Medicare reimbursement for several modalities of asynchronous communications, including asynchronous interprofessional internet consultations and remote evaluation of patient information.
Reimbursement for Interprofessional Internet Consultations (eConsults)
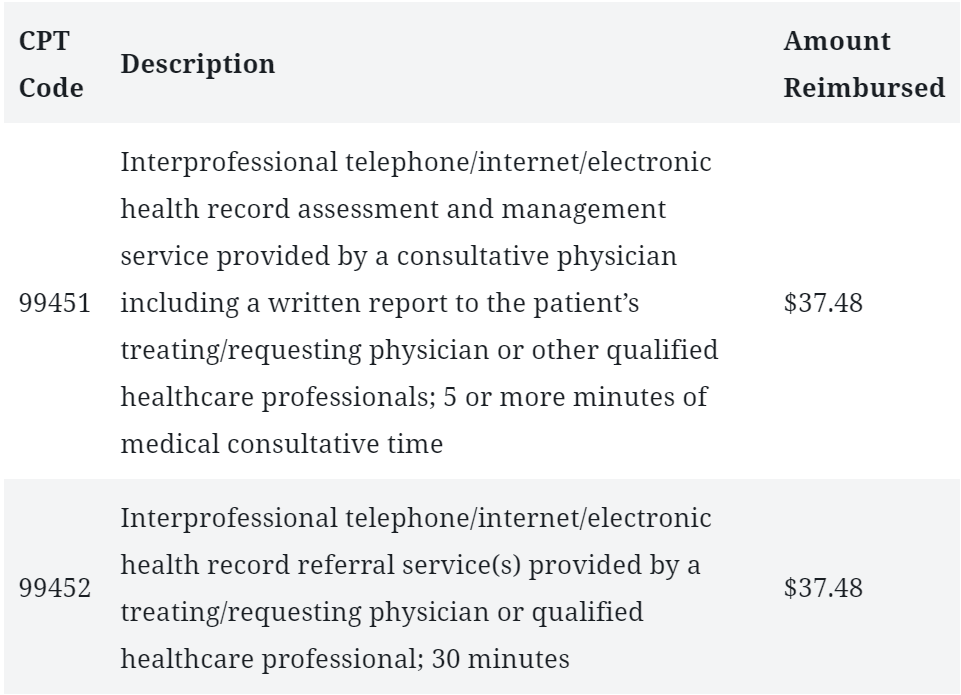
The new peer-to-peer consultation are: 99451 and 99452. The codes 99446 and 99449 existed already but were unpriced. The new fee structure includes a revised description and reimbursement. Under CPT codes 99451 and 99452, Medicare eConsults are now reimbursable under Original Medicare, and some Medicare Advantage patients may be eligible as well.
For Medicare Advantage beneficiaries, reimbursement rates may differ from those offered to Original Medicare beneficiaries. Further, the availability of reimbursement may depend on the state of residence for the patient’s plan and the provider’s contract status.
For Medicaid programs, eConsults are explicitly covered under CPT codes 99451 and 99452 in Connecticut, Kentucky, Michigan, Minnesota, Montana, Nebraska, and Utah. States, where eConsults are not covered, include Indiana, Maryland, Mississippi, Missouri, Texas, West Virginia, and the District of Columbia. All other states either have yet to release their 2019 fee schedule or do not list information about eConsult coverage.
Reimbursement for Remote Evaluation of Pre-recorded Patient Information
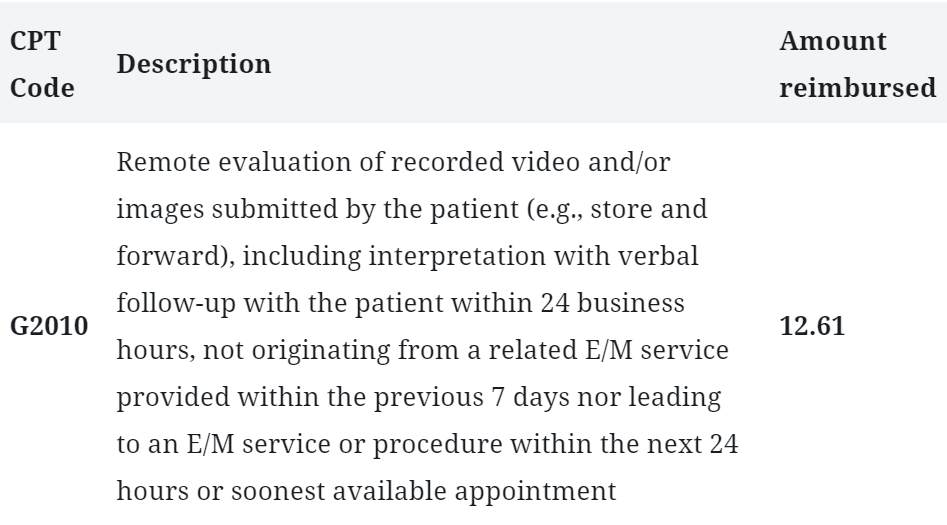
Technology for forwarding patient information via video or images has been useful in facilitating remote triage, diagnosis, and treatment. This has generally not been reimbursable under the Medicare telehealth benefit, but CMS has proposed a new code to address this: HCPCS G2010.
This reimbursement is only available for the treatment of established patients, and informed consent is required. CMS has proposed Pre-recorded Patient Information as a billable service. There are, however, two exceptions: If the patient information originates from an E/M service in the last seven days by the same treating healthcare professional, or if the information leads to an immediate (next available) in-person visit with the same healthcare professional.
In conclusion
Developments in telehealth technologies over the past several years have made great strides in improving efficiency and quality of care while benefiting patients, doctors, and healthcare systems and administrators. Even so, it’s understandable that newer, less easily understood modalities like asynchronous telehealth may lag behind in terms of adoption due to uncertainties surrounding the efficacy of and reimbursement for these services. However, the clear benefits of asynchronous telehealth technologies such as eConsults, along with recent telehealth-friendly CMS reimbursement changes, demonstrate that this modality must be factored into telehealth strategies if they are to be effective in maximizing access, efficiency, and outcomes.
About Brooke LeVasseur
Brooke LeVasseur is the CEO of AristaMD, an eConsults solution that empowers PCPs to improve specialty care access, reduce cost-of-care, improve patient outcomes, and provider satisfaction.LeVasseur has over 15 years of leadership experience launching new, innovative healthcare products and solutions to payers and providers. After graduating from Stanford University, she worked in equity research, covering medtech companies for Thomas Weisel Partners.
