Change Healthcare AI can help providers identify problem claims and prevent denials before they happen, avoiding costly rework, delays, and improving revenue flow.
Today Change Healthcare announced that it has applied its Claims Lifecycle Artificial Intelligence (AI) technology to its claims management suite with the introduction of Assurance Reimbursement Management™ Denial Propensity Scoring and Revenue Performance Advisor Denial Prevention. With performance enhanced by Claims Lifecycle AI, providers of any size can now proactively identify problem claims that could result in denials, and remediate potential issues before the claims are filed.
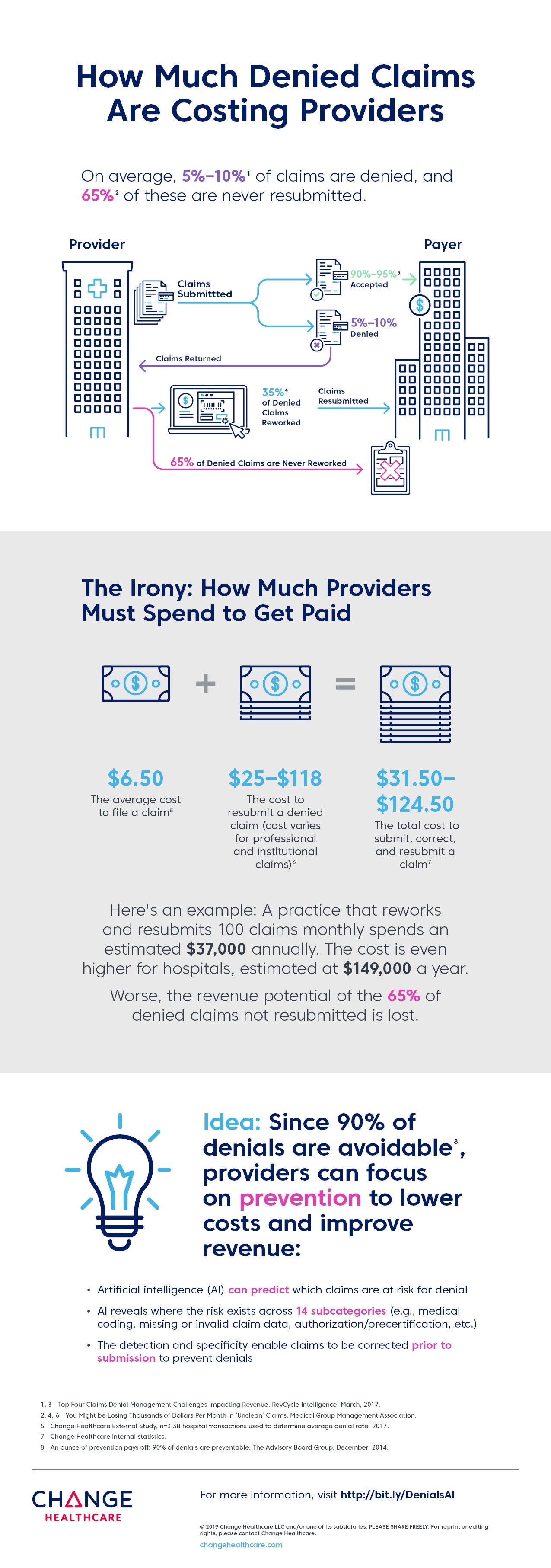
AI Could Identify & Flag Up to 35% of Denials Prior to Submission
The AI infused in these applications can now help customers predict denials, optimize claims submissions, and provide actionable recommendations that enable providers to better mitigate denials before a claim is submitted. Change Healthcare’s analysis of 2018 data spanning more than 500 million service lines showed that Change Healthcare Claims Lifecycle AI could identify and flag up to 35% of denials prior to submission. This represents $6.2 billion in forecasted allowed amounts and millions in potential administrative savings from reduced re-work and appeals.
The Change Healthcare Claims Lifecycle AI service has been trained on more than 500 million service lines making up over 205 million unique de-identified claims data, which were de-identified consistent with customer contracts and applicable laws, that touch $268 billion in charges, which is unparalleled in its scope. The service leverages the company’s Intelligent Healthcare Network data from more than 2,200 payers, 5,500 hospitals/health systems, and across 900,000 physicians.
Claims Lifecycle AI for denials is now activated within Change Healthcare’s claims management suite, including Assurance Reimbursement Management (for hospitals and health systems, billing services, and other providers) and Revenue Performance Advisor (for physician practices, labs, home health, medical billing services vendors, and other providers). These solutions address the claims management needs for the entire provider ecosystem—from small to large practices, laboratories, durable medical equipment providers, and nursing homes up to hospitals and health systems.
Additionally, channel partners using the Intelligent Healthcare Network from Change Healthcare will be able to access these new claims management capabilities via the Change Healthcare API Marketplace.
Why It Matters
“This is the first application of artificial intelligence to predict and reduce denials that operates at scale,” said Marcy Tatsch, senior vice president and general manager, Revenue Cycle Management, Change Healthcare. “Bringing all of these capabilities together and preventing a significant burden is a real game-changer for revenue cycle management, which, until now, has been a more retroactively focused process.”