Editor’s Note: D’Arcy Guerin Gue is a co-founder of Phoenix, with over 25 years of experience in executive leadership, strategic planning, IT services, knowledge leadership, and industry relations — with a special focus on patient engagement and federal compliance issues. She currently serves as the Director of Industry Relations at Phoenix Health Systems, a division of Medsphere Systems
In the public mind, the needs of the mentally ill and addicted have always taken a backseat to those of the physically ill and injured. This dichotomy was never more obvious than when behavioral health and addiction providers were excluded from the Meaningful Use program created by the American Recovery and Reinvestment Act (ARRA) of 2009.
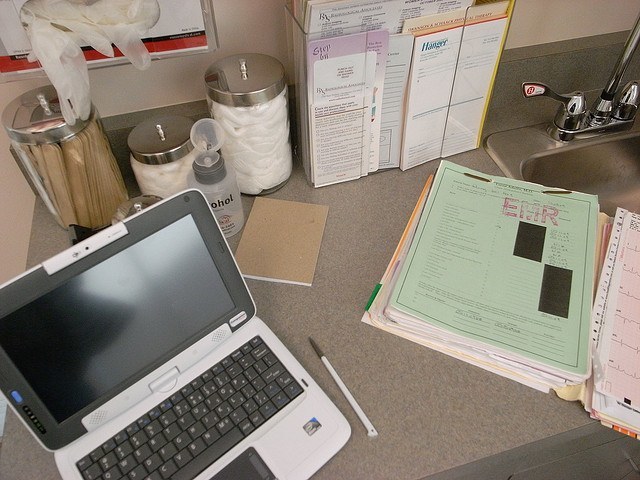
Predictably, EHRs have proliferated among incentivized providers and remain comparatively rare with behavioral health and addiction organizations. As of December 2015, 98 percent of eligible hospitals and nearly 60 percent of office-based physicians had implemented an EHR, according to HealthIT.gov. All told, these providers received over $32 billion in federal tax dollars to cover EHR-related costs.
Contrast those numbers with the relatively few behavioral health and addiction providers that have EHRs. The National Council for Behavioral Health reported in 2012 that fewer than 30 percent had one. A 2012 Health Affairs study said only 21 percent of psychiatric hospitals had EHRs. Software Advice’s 2014 study of 385 mental health software buyers found that most were from small practices; only 16 percent represented organizations with more than 11 doctors.
Now, seven years after ARRA, healthcare leaders are increasingly worried about the EHR divide between acute and mental health care. Clinicians know that physical and mental health are inextricably connected; without the ability to share care data across patient populations, comprehensive care and treatment is an unreachable goal, putting the health of millions of Americans at stake. While HIMSS, AHA, NAPHS, CMS, Congress and others have discussed these problems and proposed various solutions, financial support for EHR adoption by behavioral health and addiction providers remains elusive.
And yet, even without Meaningful Use, an increasing number of behavioral health hospitals are blazing their own trails toward better care through EHRs. In-depth interviews with leaders of three such organizations illustrate why and how they made this transition, and how working with an EHR has proved beneficial to patient care.
– IntraCare North is a 90-bed psychiatric hospital managing two care facilities in the Houston, Texas, area. IntraCare offers a continuum of inpatient and outpatient mental health and chemical dependency services to children, adolescents and adults.
– The Recovery Center at EvergreenHealth Monroe, based in Monroe, Washington, offers a multidisciplinary treatment team that provides inpatient and outpatient services for substance abuse patients throughout the Pacific Northwest. It is licensed for 32 beds.
– Silver Hill Hospital is a psychiatric hospital with 129 licensed beds. Located in New Canaan, Connecticut, the independent not-for-profit facility provides inpatient and residential transitional living programs for adolescents and adults. Its 45-acre campus includes ten buildings designated for different levels of care.
All three organizations in this study shared an upfront advantage: Each had leaders and staff that were familiar with EHRs and astute enough to observe how these systems could change the healthcare landscape. Previous interactions with acute care providers gave them valuable insight regarding the potential benefits of EHRs: better quality measurement, improved internal processes, simplified reporting, integrated care management and more accurate patient records, to name but a few. Leaders of these organizations each provided answers to the same four questions.
1. From Paper to Electronic: Why take this giant step?
Better Record Keeping and Reporting
“We knew moving to an EHR would provide a better quality record because EHRs don’t allow skipping over data fields, which often can happen in a paper record,” explained IntraCare CEO of Healthcare Operations Terry Scovill. “Moreover, online records can be monitored internally far more easily.” Scovill also noted that the simple illegibility of paper records and high costs of paper were problems that could be virtually eliminated with electronic data entry. “Staff therapists and nurses were doing so much time-consuming documentation,” added Eric Britt, an EvergreenHealth supervisor. “We knew typing would be more accurate and productive once they became accustomed to it.” IntraCare leaders also wanted to minimize the paperwork burden of reporting to the Joint Commission and state and federal agencies. “Tracking down needed records and being able to read them was a big problem that detracted from our central mission,” according to IntraCare Project Manager Phyllis Qualls.
Immediate Access to Patient Records
For Silver Hill, trying to manage documentation across ten buildings and multiple treatment programs was frustrating, so instant access to patient records was essential. “Discharge from one program to another on paper was a nightmare,” said Silver Hill President and Medical Director Sigurd Ackerman, M.D. “Clinical records were hard to find … to operate more smoothly, our staff needed immediate access to the whole patient record.” EvergreenHealth Medical Director John Patz, M.D., agreed. “Multiple access was needed, as was the ability to easily audit records. We wasted too much time hunting down records that lived on one piece of paper.”
Integrated and Improved Care
Leaders and staff from all three hospitals expected a comprehensive EHR to enable better care integration with other providers.
“IntraCare wanted the ability to easily share patient information with referrals, which was difficult to do with paper records,” Scovill explained. “We knew that if we could quickly share quality data with referring physicians, everyone would benefit, especially our patients.”
For key hospital staff, an EHR gave them the ability to quickly understand a patient’s care history and rapidly determine correct next steps.
“We expected electronic patient record sharing to help us better serve our patients by minimizing medication delays and inaccuracies—critical in a substance abuse program,” said Dr. Patz.
