What You Should Know:
- Waystar (Nasdaq: WAY), a provider of leading healthcare payment software, today announced the launch of Waystar AltitudeAI™, a comprehensive set of AI capabilities for providers, including AltitudeCreate™, a new generative AI innovation focused on appealing denied claims.
- By autonomously generating appeal letters, Waystar aims to help providers recover a substantial portion of payments tied to more than 450 million annually denied claims, ultimately enabling
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
Q/A: Cedar Exec Talks The Untapped Potential of AI in Healthcare Call Centers in 2025
What if AI could dramatically reduce call volume, improve patient satisfaction, and empower your call center staff? In this exclusive interview, Dugan Winkie, Head of Commercial Strategy at Cedar, sheds light on the often-overlooked opportunity of leveraging AI in healthcare call centers.
Winkie explores the unique challenges and opportunities AI presents for providers, highlighting the potential for increased efficiency, improved patient experiences, and significant financial gains. He
Read More
The RCM Arms Race: How AI is Reshaping Healthcare Finance in 2025
As healthcare providers head into 2025, a technological arms race is reshaping revenue cycle management (RCM), with artificial intelligence (AI) emerging as the decisive factor between financial success and struggle. With approximately 46% of hospitals and health systems already utilizing AI in their RCM operations, the industry stands at a critical juncture where matching payer sophistication has become imperative for survival. This transformation represents a fundamental shift in how
Read More
Why the CFPB Medical Debt Credit Reporting Ban Could Hurt More Than It Helps
The Consumer Financial Protection Bureau (CFPB) has announced that it wants to ban the inclusion of medical debt data in credit reports to lessen the negative impact of medical debt on credit scores and improve financial outcomes for consumers.
Though well-intentioned, the CFPB's medical debt credit reporting ban would severely inhibit the activities of medical collection companies who partner with healthcare providers to collect outstanding medical accounts. It also could have
Read More
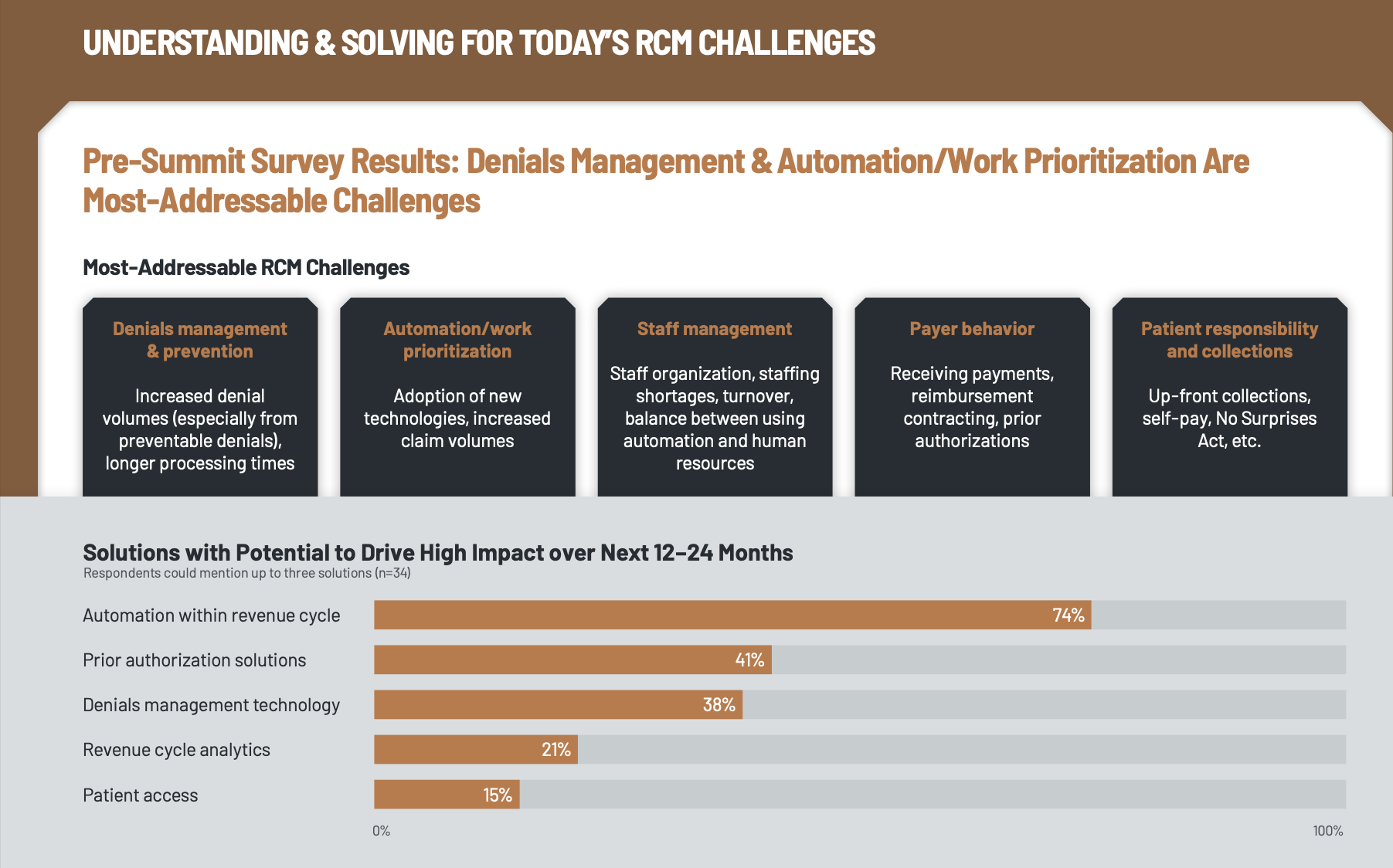
KLAS Revenue Cycle Management Summit 2024: Top Challenges and Solutions
What You Should Know:
- The KLAS Revenue Cycle Management Summit 2024 brought together 117 revenue cycle management (RCM) leaders to address pressing challenges, explore emerging technologies, and enhance cybersecurity in healthcare.
The KLAS Revenue Cycle Management Summit provided healthcare leaders navigating the evolving RCM landscape with practical solutions and best practices for optimizing revenue cycle operations.
Top RCM Challenges and Solutions
Summit attendees
Read More
CentralReach Launches 2 AI Solutions to Maximize Clean Claims
What You Should Know:
- CentralReach, a provider of Autism and IDD care software, is transforming revenue cycle management (RCM) with the launch of two innovative AI-powered solutions: CR ClaimCheckAI™ and the upcoming CR ClaimAgentAI™.
- The AI tools address critical challenges faced by ABA and multidisciplinary organizations, such as increasing profitability and optimizing cash flow, despite staffing shortages and financial constraints.
CR ClaimCheckAI: Intelligent Claims
Read More
Aspirion Acquires Boost Healthcare to Enhance RCM Capabilities
What You Should Know:
- Aspirion, a provider of healthcare technology revenue cycle management (RCM) solutions, today announced the acquisition of Boost Healthcare, a revenue cycle firm that joins revenue cycle leaders on their journey to improve their organization’s financial performance. Financial details of the acquisition were not disclosed.
- The strategic acquisition strengthens Aspirion's commitment to helping healthcare providers secure accurate and timely reimbursement for
Read More
4 Cornerstones for Successful AI Implementation in Hospital Revenue Cycle Management in 2025
In recent years, payers have increasingly turned to artificial intelligence (AI) as a tool to streamline claims processing, accelerating the deployment of rules related to prior authorizations and medical-necessity assessments. Providers believe this has been a key driver behind a corresponding surge in claims denials, as well funded payers leverage technology to rapidly render these determinations and send them back to hospitals.
This trend has providers looking to respond with a
Read More
Cofactor AI Nabs $4M to Combat Hospital Claim Denials with AI
What You Should Know:
- Hospitals across the country are facing an ever-increasing onslaught of claims denials from insurance companies, with denials up 20.2% in 2023, according to the American Hospital Association. These denials – triggered by AI and often error-prone – cost hospitals $20 billion a year in administrative bloat and reduce patients’ access to quality care.
- To help hospitals fight back, Cofactor AI today introduced a new first-of-its-kind AI-powered
Read More
Revitalizing Medicare Advantage: How The Push to Streamline Prior Authorization Will Impact Senior Care
As a physician, the odds that you’ve had a negative experience related to the prior authorization process are (unfortunately) highly likely. According to the American Medical Association’s (AMA) 2023 Prior Authorization Physician Survey, 1 in 4 physicians report that prior auths “have led to a serious adverse event for a patient in their care.” Think about the toll that this takes on professionals whose primary job is providing lifesaving care, and the thing preventing this care is outside their
Read More