What You Should Know
The Deal: RevSpring (backed by Frazier Healthcare Partners) has acquired TrustCommerce (a portfolio company of Waud Capital Partners) to build a dominant, end-to-end healthcare payment platform.The Tech: TrustCommerce brings its enterprise gateway connectivity and deep integrations with major Electronic Health Records (EHRs). This allows RevSpring to offer a seamless, unified payment stack from the front desk to the back office.The "BYOM" Advantage: A major strategic
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
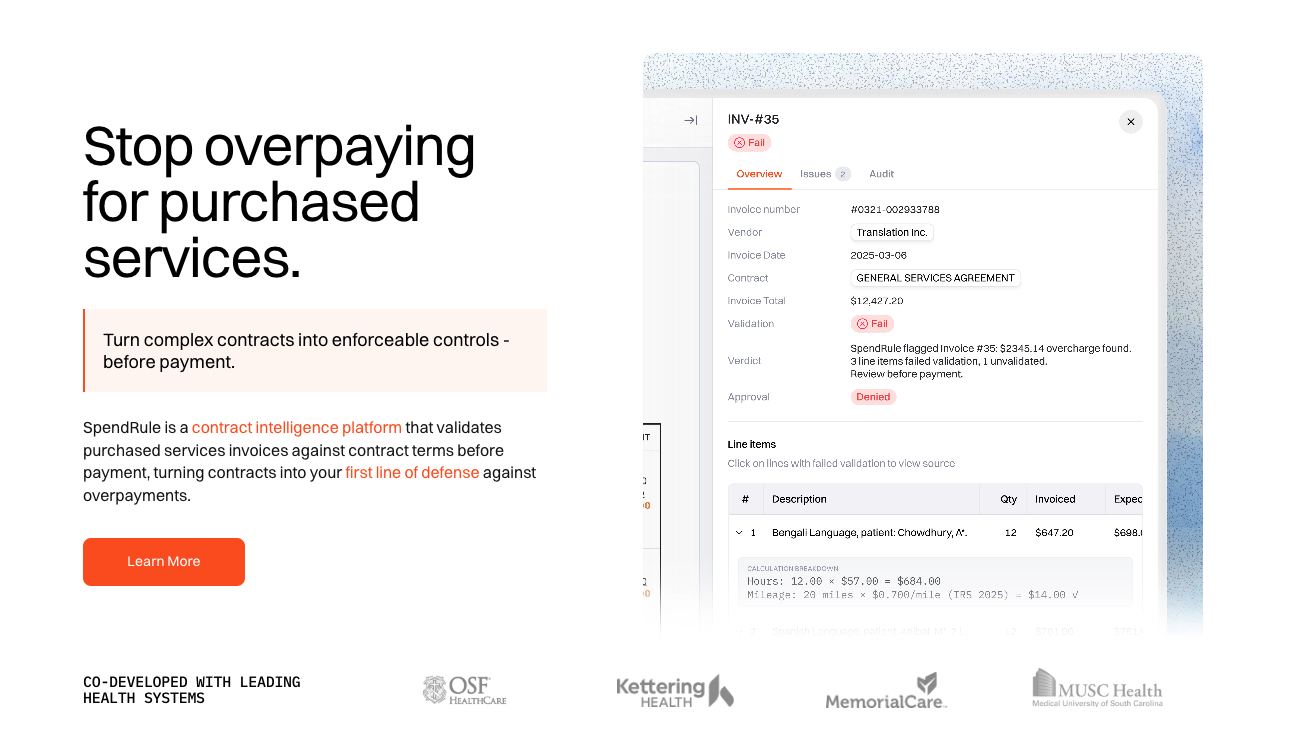
SpendRule Launches AI-Powered Contract Intelligence Platform with OSF HealthCare and MemorialCare
What You Should Know
The Launch: SpendRule has officially launched its AI-powered contract intelligence platform, backed by investors like Abundant Venture Partners and MemorialCare Innovation Fund.The Problem: "Purchased Services" (non-labor spend like housekeeping, IT, and food service) represent a $323 billion category where hospitals often overpay due to complex contracts. Industry estimates suggest $32 billion is wasted annually on preventable overpayments.The Solution: SpendRule
Read More
Ambience Healthcare Launches “Chart Awareness” to Automate Coding and Clinical Summaries
What You Should Know
The Leap: Ambience Healthcare has launched "Chart Awareness," a capability that allows its AI to interpret a patient’s full longitudinal record (labs, imaging, prior notes) rather than just transcribing the current conversation.The Features: The update includes Chart-Aware Patient Summaries, Diagnostics (auto-extracting lab trends), and Coding (substantiating complex codes like G2211 based on patient history).The Proof: In a head-to-head evaluation at MultiCare Health
Read More
Midstream Health Partners with CommonSpirit Health to Deploy AI Financial Operations Platform
What You Should Know
The Deal: Midstream Health, a platform backed by Andreessen Horowitz (a16z), has secured a strategic partnership with CommonSpirit Health. The health system isn't just a customer; its venture arm is an initial investor.The Tech: Midstream deploys "AI Agents" that scour financial data to find lost value. Unlike standard analytics, these agents are "contract-aware," proactively flagging missed rebates, pricing errors, and underpayments that humans miss.The Impact: The
Read More
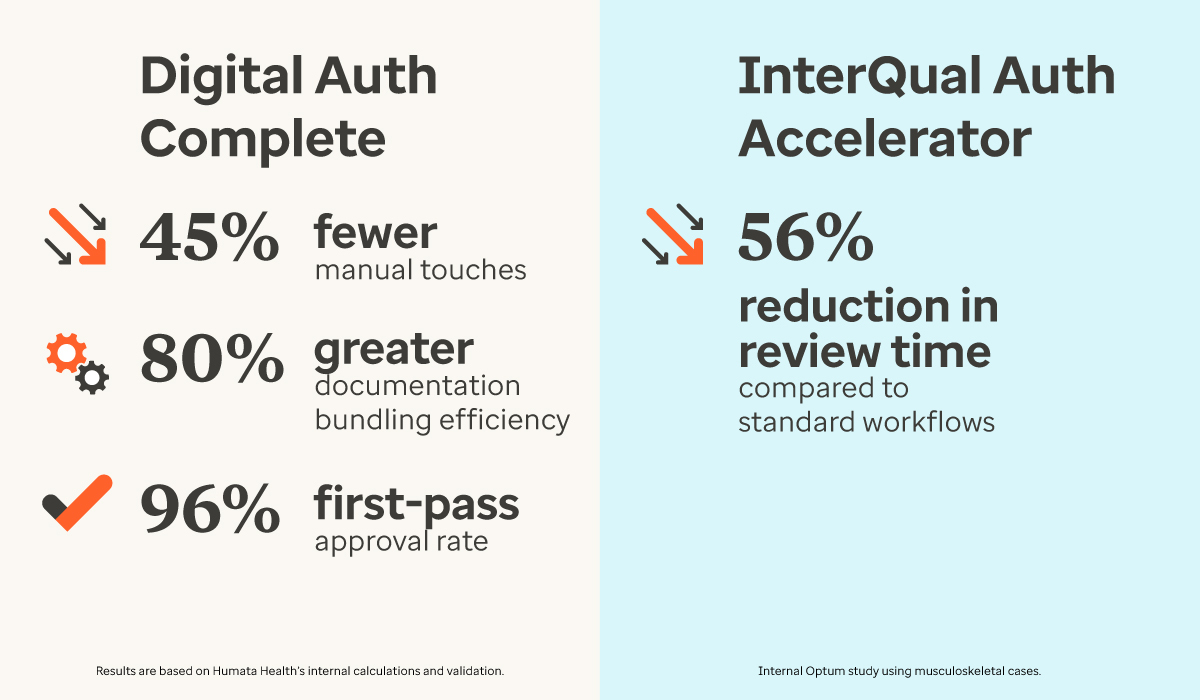
Optum Launches AI Platform to Erase Prior Auth Friction
What You Should Know
The Launch: Optum is rolling out a dual-sided AI strategy to modernize prior authorization: Digital Auth Complete for providers (powered by Humata Health) and InterQual® Auth Accelerator for payers.The Provider Impact: By embedding AI directly into the EHR, the provider-side tool has demonstrated a 96% first-pass approval rate in early deployments, aiming to reclaim the average 13 hours per week staff spend on these tasks.The Payer Impact: The payer-side solution focuses
Read More
Alaffia Health Raises $55M to Fix Claims Waste with “Agentic AI”
What You Should Know
The Funding: Alaffia Health has raised a $55M Series B led by Transformation Capital, bringing its total funding to over $73M.The Tech: The company uses "Agentic AI"—autonomous software paired with human clinicians—to forensically audit medical claims against patient records, targeting the estimated $570 billion in annual administrative waste.The ROI: Unlike "black box" automated solutions, Alaffia’s transparent model has already saved health plans over $100M, delivering
Read More
The $1.9B Exit: Why CommonSpirit is Insourcing Revenue Cycle and Tenet is Betting Big on Conifer AI
What You Should Know
The Deal: Tenet Healthcare and CommonSpirit Health are unwinding their partnership regarding Conifer Health Solutions. CommonSpirit will pay Tenet approximately $1.9 billion over three years, while Conifer will redeem CommonSpirit's 23.8% equity stake for $540M.The Shift: CommonSpirit has decided to insource its revenue cycle operations starting in 2027. Conifer will continue to provide services through the end of 2026 to ensure a smooth transition.The Forecast: Alongside
Read More
NuvemRx Acquires par8o 340B Referral Capture Business from R1 RCM
What You Should Know
The Deal: NuvemRx has acquired the 340B referral capture business of par8o (formerly owned by R1 RCM), effectively consolidating two major players in the safety-net pharmacy space.The Scale: The combined entity now supports over 800 covered entities nationwide, representing a cumulative patient base of 70 million lives.The Tech: The acquisition integrates par8o’s referral technology with NuvemRx’s platform, reportedly using AI to automate up to 85% of the complex referral
Read More
Kodiak Solutions Acquires BESLER to Close the “Revenue Leakage” Gap
What You Should Know
The Deal: Kodiak Solutions has acquired BESLER & Company, integrating a 40-year veteran of revenue recovery into its modern analytics platform.The Tech Synergy: The acquisition adds BESLER’s specialized Transfer DRG software—used to detect Medicare underpayments—to Kodiak’s broader net revenue reporting suite.The Strategy: This is a "platform play." Kodiak is consolidating niche revenue cycle tools under one roof, allowing hospital CFOs to replace fragmented point
Read More
The Self-Driving Revenue Cycle: Claim Health Raises $4.4M to Fix Post-Acute Care’s Biggest Bottleneck
What You Should Know
The News: Claim Health has raised a $4.4 million Seed round led by Maverick Ventures to scale its "AI-native" revenue operations platform for post-acute care.The Traction: Since exiting Y Combinator’s Spring 2025 batch, the company has grown revenue 30x in under a year, driven by providers seeking to replace legacy manual workflows.The Tech: The platform offers a "self-driving" revenue cycle—automating everything from patient intake to payment reconciliation—delivering a
Read More