What You Should Know
The Launch: Optum is rolling out a dual-sided AI strategy to modernize prior authorization: Digital Auth Complete for providers (powered by Humata Health) and InterQual® Auth Accelerator for payers.The Provider Impact: By embedding AI directly into the EHR, the provider-side tool has demonstrated a 96% first-pass approval rate in early deployments, aiming to reclaim the average 13 hours per week staff spend on these tasks.The Payer Impact: The payer-side solution focuses
Read More
Prior Authorization
Abridge and Availity Partner to Automate Prior Authorization at the Point of Conversation
What You Should Know
- Abridge, the leader in clinical conversational AI, and Availity, the nation’s largest health information network, have launched a first-of-its-kind collaboration to automate prior authorization in real-time.
- By embedding Availity’s FHIR-native Intelligent Utilization Management solution into Abridge’s Contextual Reasoning Engine, the partnership aims to provide clinicians with visibility into coverage requirements and enable payer determinations during the
Read More
Why Faster Prior Authorizations Won’t Fix Healthcare’s Real Issues
Few phrases raise blood pressure among doctors and patients like “prior authorization.” Ask any clinician and you’ll hear the same story: delayed treatments, endless back-and-forth, and vulnerable individuals left waiting while paperwork wins the day.
For providers, prior authorizations are a constant drain of time and energy. For patients, they can mean worsening conditions, missed windows for effective treatment, or even care that never arrives at all. And for payers, prior
Read More
AI Prior Authorization: Humata Health Partners with CMS on WISeR Model to Modernize Medicare
What You Should Know:
- Humata Health, a provider of AI-powered prior authorization technology, has been selected by the Centers for Medicare & Medicaid Services (CMS) as a key partner for its new initiative: the Wasteful and Inappropriate Service Reduction (WISeR) model.
- CMS, the single largest payer for healthcare in the U.S., has chosen Humata Health to deploy its proprietary technology in a program that directly addresses the staggering variability of care and significant
Read More
SPRY PT Launches AI-Powered Prior Authorization Solution to Automate 80% of Workflow
What You Should Know:
- SPRY PT today unveiled the industry’s first AI-powered Prior Authorization & Eligibility solution, proven to automate 80% of the prior authorization workflow while ensuring 100% of authorizations are completed through a combination of AI automation and expert review.
- The solution reduces related denials by up to 75%, streamlines workflows across major payers including Carelon/BCBS, UnitedHealthcare, and Humana, and provides unlimited, real-time eligibility
Read More
Oracle Health to Launch AI-Powered Solutions for Payers and Providers
What You Should Know:
- Oracle Health has unveiled a new strategy to strengthen the collaboration between healthcare providers and payers.
- The company plans to introduce a comprehensive suite of AI-powered apps and agents designed to automate prior authorizations, reduce claims denials, and improve care coordination. These solutions aim to significantly cut down on administrative costs, which are estimated at approximately $200B annually, and enhance value-based care
Read More
HHS Regulatory Breakthrough to Streamline Prior Authorizations and Improve Drug Price Transparency
What You Should Know:
- The U.S. Department of Health and Human Services (HHS) has announced a new regulatory reform that will give doctors and patients real-time access to prescription drug information.
- The rule, which takes effect on October 1, will allow millions of Americans for the first time to compare drug prices, view out-of-pocket costs, and access prior authorization requirements. The reform aims to help them identify the most cost-effective treatments and prevent
Read More
Inovalon and Google Cloud Partner to Launch AI-Enabled Prior Authorization Solution
What You Should Know:
- Inovalon, a provider of solutions that empower data-driven healthcare, has announced a new collaboration with Google Cloud to develop an AI-enabled solution designed to address administrative burdens in the healthcare industry.
- The partnership will combine Inovalon’s extensive data solutions and subject matter expertise with Google Cloud's advanced AI and machine learning capabilities to tackle time-consuming prior authorization processes.
A Vision for
Read More
ZeOmega Partners With Datycs to Optimize Prior Authorization
What You Should Know:
-ZeOmega®, the leading population health management organization, today announced its partnership with Datycs, a leading provider of clinical AI/Natural Language Processing (NLP) solutions, to automate converting unstructured data from faxed documents into standardized, interoperable, and actionable information.
- The collaboration will help health plans garner insights that will drive improvements in member care, provider and payer workflows, and overall
Read More
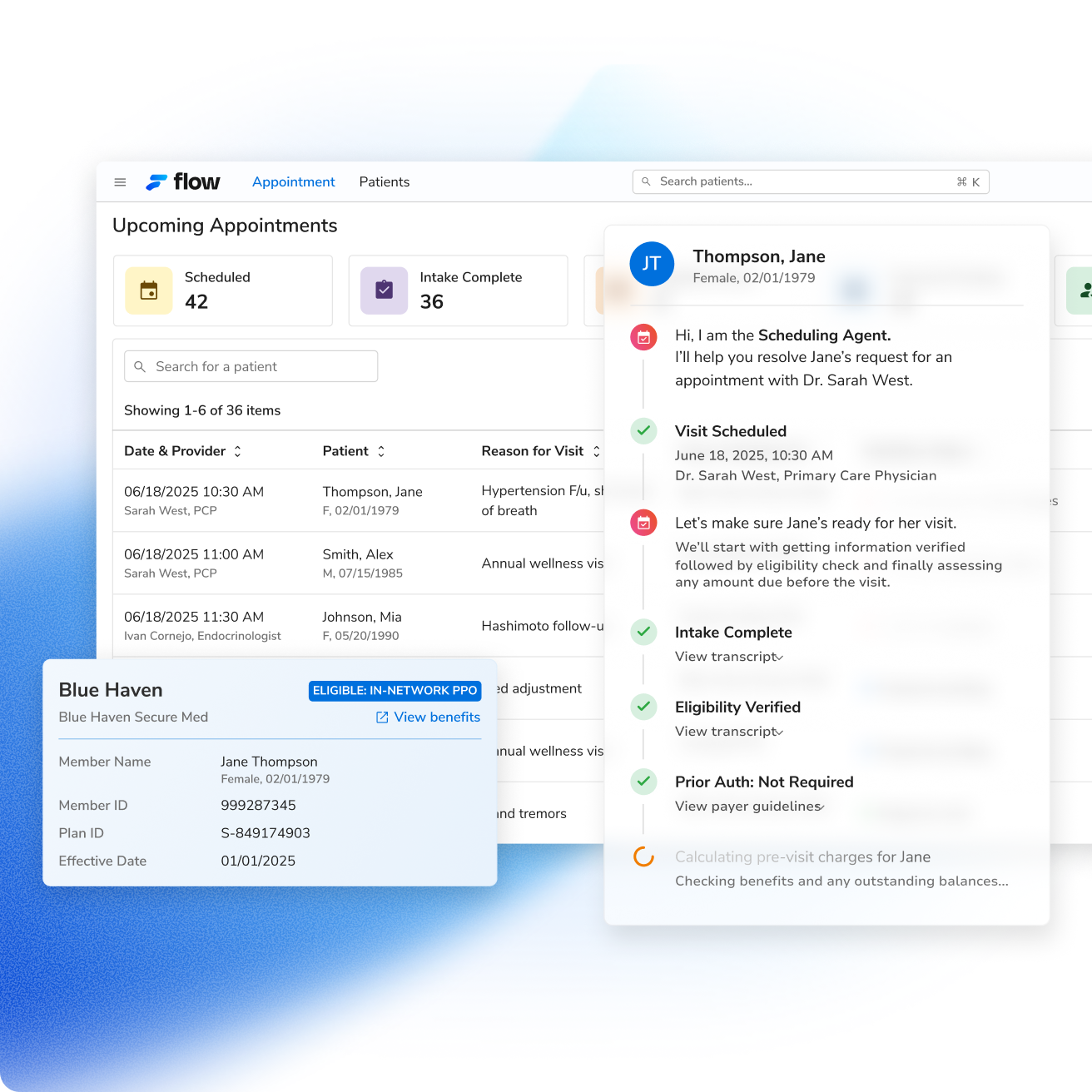
Innovaccer Launches AI-Powered Prior Authorization Solution: Flow Auth
What You Should Know:
- Innovaccer Inc., a healthcare AI company launches Flow Auth, a new AI-powered prior authorization solution.
- As part of the company's revenue cycle performance platform, Flow by Innovaccer, Flow Auth is designed to automate the entire prior authorization (PA) workflow, helping healthcare organizations accelerate care delivery and optimize revenue capture.
- Innovaccer projects that the solution could lead to a 50% reduction in the time clinicians
Read More