What You Should Know:
– A new evaluation from the Peterson Health Technology Institute (PHTI) has assessed the effectiveness of virtual solutions for opioid use disorder (OUD).
– The report reveals that while these solutions are as effective as traditional, in-person care, they only provide a modest improvement in patient outcomes and do not appear to be significantly expanding access to treatment.
Modest Clinical Benefits, Unclear Economic Impact
According to the PHTI evaluation, virtual OUD solutions help patients stay in treatment an average of 13 more days over six months compared to usual care. Treatment retention is considered a critical factor for clinical effectiveness, as patients who remain in care have a lower risk of fatal overdose and fewer emergency department visits and hospital admissions. While any additional time in treatment is beneficial, the report suggests that this modest improvement is not enough to substantially reduce overall healthcare spending. In fact, digital wraparound solutions, which are added to usual care, may even increase costs because the price of the solution can exceed the savings from improved treatment retention.
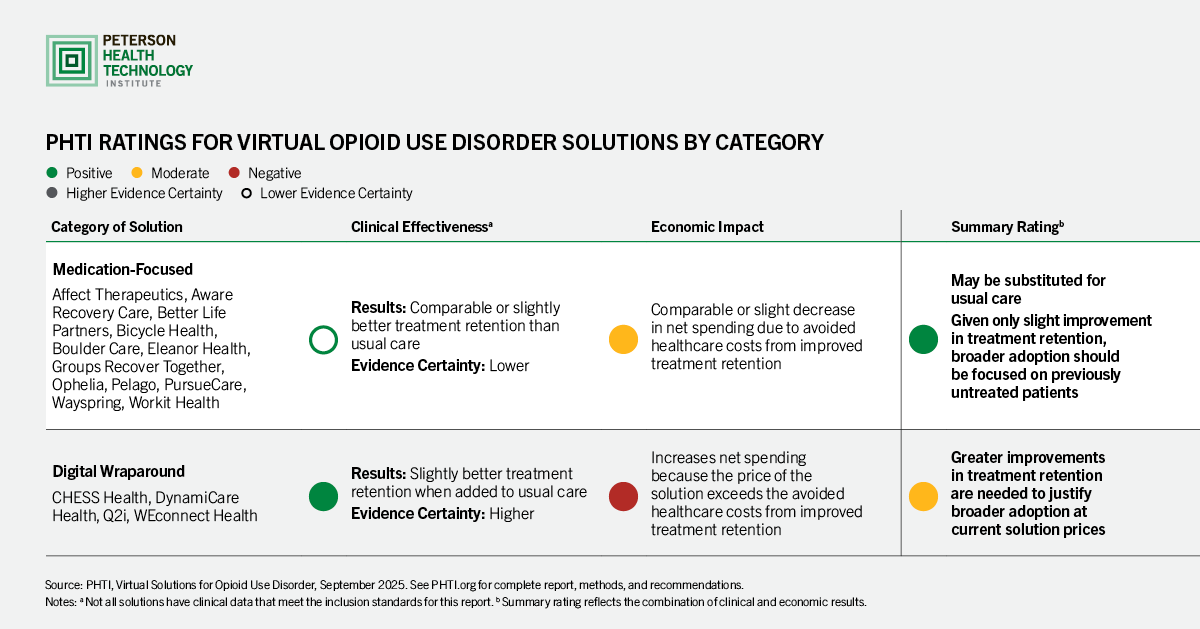
PHTI evaluated two main categories of virtual OUD solutions:
- Medication-focused solutions: These solutions offer virtual prescribing, primarily for buprenorphine, with optional support services. PHTI found that these solutions can be a substitute for traditional care, with comparable or slightly lower costs for payers due to a reduction in hospitalizations and emergency room visits.
- Digital wraparound solutions: These solutions are added to existing treatment programs and offer services such as contingency management and peer support. The evaluation found that these solutions increase net spending for purchasers because their cost is higher than the avoided healthcare costs from improved retention.
The Access Gap and Recommendations for the Future
Despite the expectation that virtual solutions would increase the number of people in medication-based OUD treatment, the assessment found no evidence that these solutions are disproportionately enrolling new patients. Currently, virtual solutions primarily reach individuals who are already in some form of treatment or would have sought in-person care.
To address this and other ongoing challenges, the PHTI report provides several recommendations:
- Advance the evidence: More research is needed to determine which aspects of virtual OUD solutions are most effective and for which patient populations.
- Expand access: Innovators should focus on strategies to engage and bring more untreated patients into care and keep them in treatment longer.
- Modernize policy: Policymakers should modernize teleprescribing and licensure rules to enable these programs to expand into underserved areas. This includes finalizing proposed DEA rules for a special teleprescribing registration for controlled substances.
- Leverage opioid settlement funds: States and localities can use opioid abatement funds to invest in virtual OUD solutions and support evidence generation.
“When it comes to opioid use disorder, any additional time in treatment helps patients avoid relapse and overdose risk. Virtual solutions perform as well as or slightly better than traditional care models, but healthcare providers and digital solutions need to continue striving for interventions that deliver more substantial improvements in retention and effectiveness,” said Caroline Pearson, executive director of PHTI. “In the meantime, the biggest impact for these solutions is to expand adoption to previously untreated patients who can benefit from proven medications and desperately need the help.”
