What You Should Know:
– Reveleer, in partnership with Mathematica and The Harris Poll, has released the 2025 State of Technology in Value-Based Care (VBC) Report. The report’s findings come at a pivotal time, highlighting that while payer and provider alignment on VBC goals is stronger than ever, persistent gaps in technology and execution are stalling progress.
– The report is based on a national survey of 203 payer and provider decision-makers conducted from May 27 to June 10, 2025. It reveals that despite widespread agreement on the importance of technology for VBC, significant barriers such as fragmented data strategies, inconsistent AI adoption, and insufficient staff training are limiting the ability to scale improvements in care.
Payer and Provider Alignment: A Shared Vision, Fragmented Execution
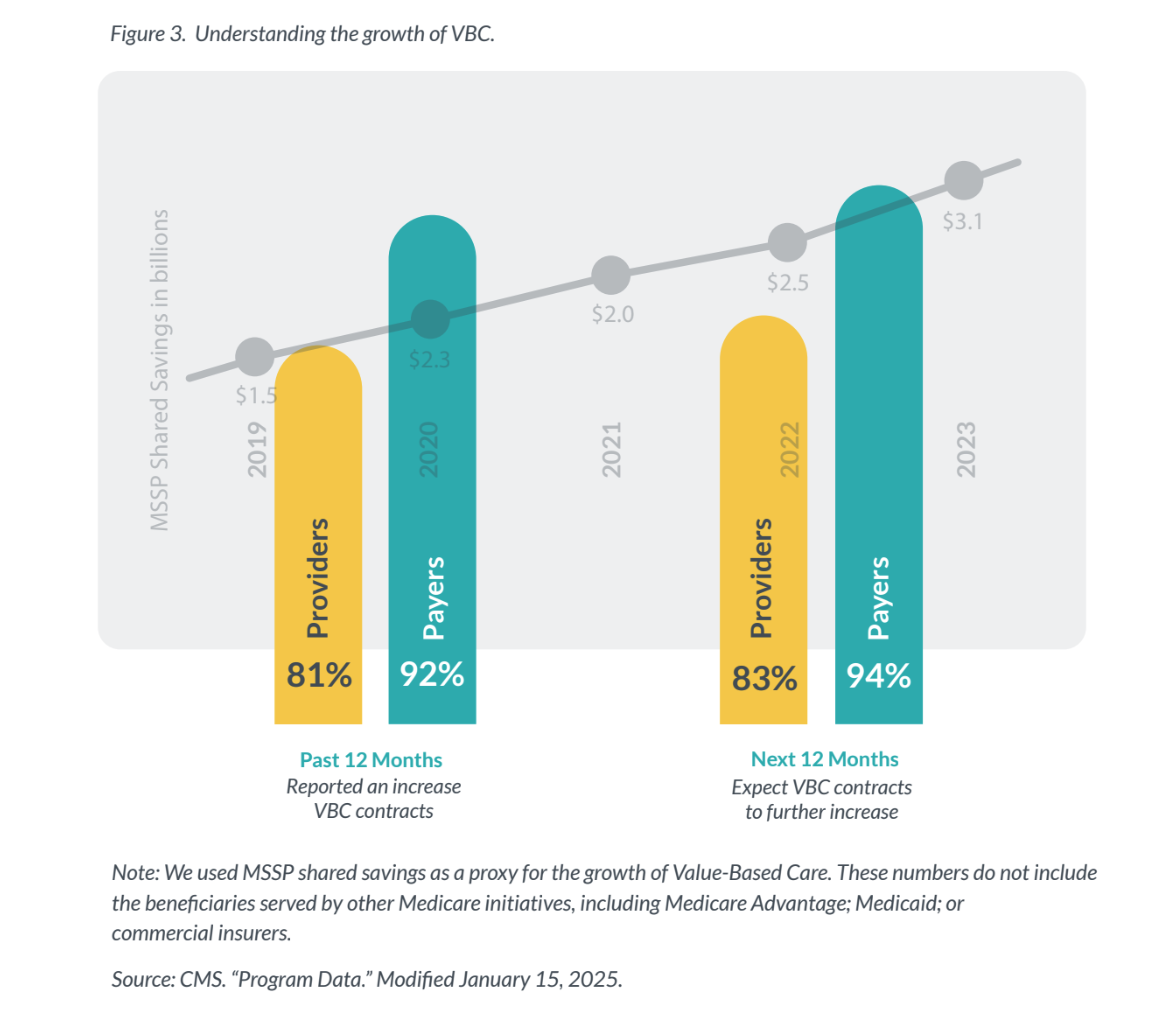
The report’s findings challenge the common industry narrative of payer-provider misalignment. In fact, 100% of providers and 97% of payers surveyed agree that their VBC goals are strongly aligned. The report suggests that the problem is not a lack of shared vision, but a lack of synchronized execution. Despite this, VBC momentum continues to grow, with 92% of payers and 81% of providers reporting an increase in VBC contracts in the past 12 months. Even more expect future growth.
“To realize the full potential of value-based care, payers and providers must collaborate at scale,” said Jay Ackerman, CEO of Reveleer. “The good news is payers and providers are finally rowing in the same direction. But if they don’t row in sync, we won’t move forward. This report points to a clear call to action: the alignment is there and the tools are ready. Tighter collaboration and true transformation are within reach.”
The Data Disconnect
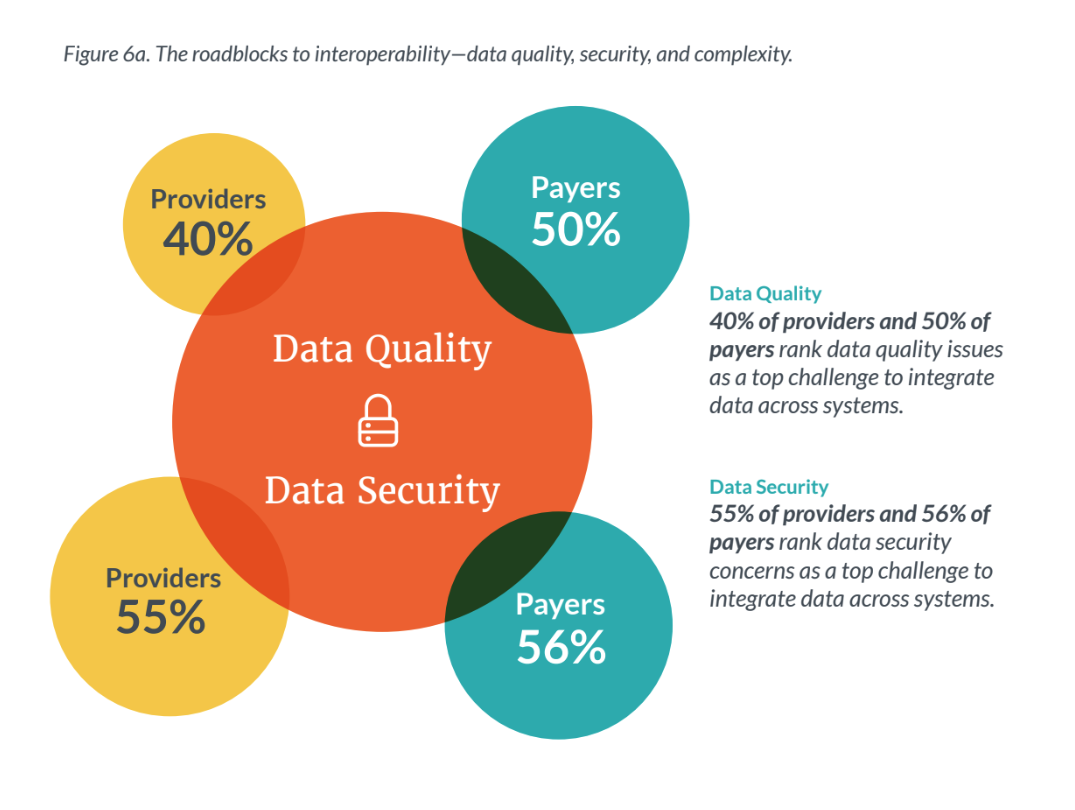
Data management is a known strategic advantage, with 97% of providers and 96% of payers agreeing that a strong data management approach gives them a competitive edge. However, this confidence masks significant operational fragmentation.
Only about one-third of providers (33%) and payers (31%) rate their data integration capabilities as “excellent”. Furthermore, only about half of leaders (46% of providers and 53% of payers) are very confident in the accuracy and completeness of the patient data they use in VBC initiatives. This gap between expectation and reality creates a major vulnerability in effectively and safely scaling VBC.
AI Adoption: Widespread Use, Inconsistent Commitment
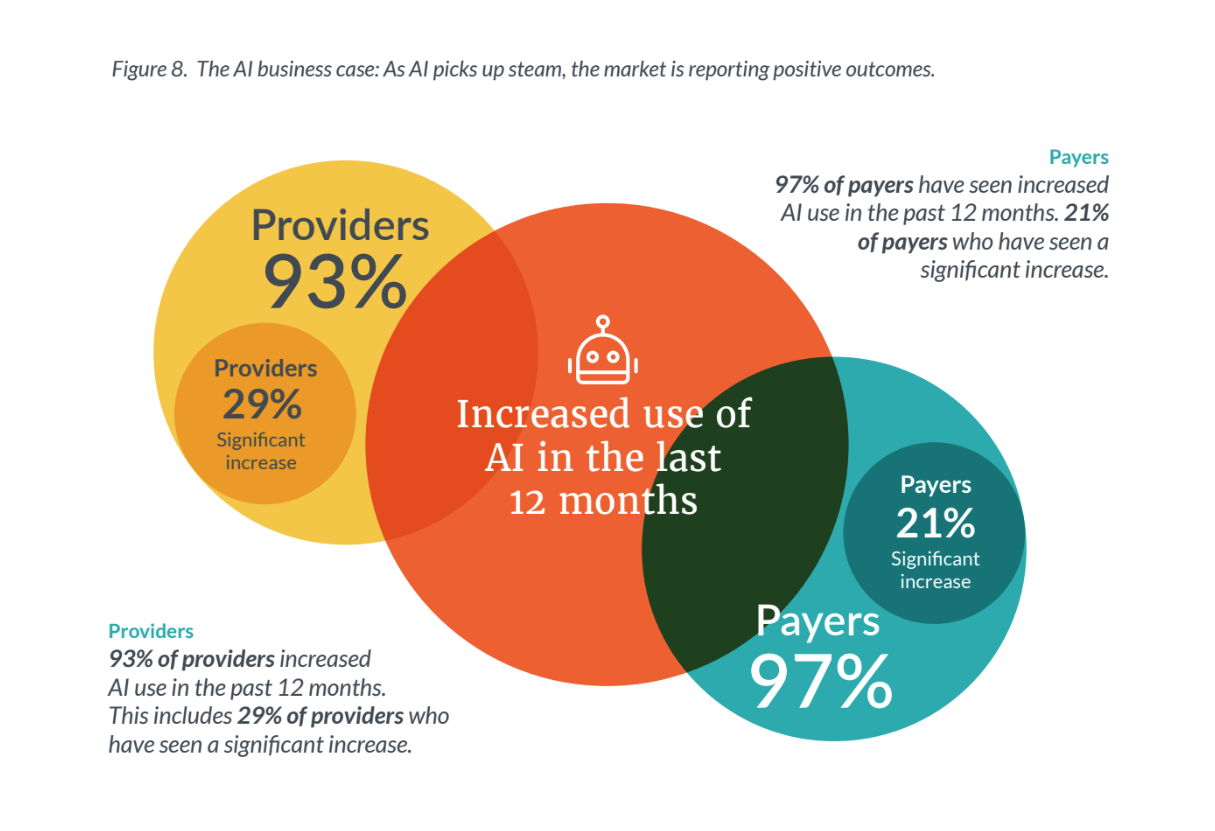
The report found that every surveyed payer and provider organization reports using AI to some degree. A majority of both groups agree that their AI approach has provided a competitive advantage , with over 80% seeing positive impacts on clinical decision-making, operational efficiency, and patient outcomes.
However, this enthusiasm has not translated into full commitment. Only 38% of providers and 40% of payers say they are “fully committed” to AI adoption. Just 29% of providers and 21% of payers have seen a significant increase in AI use in the past year. Underlying this hesitation are concerns about AI hallucinations and a lack of transparency and ethical oversight.
Training Gaps and a Call to Action
A key finding is the underinvestment in workforce readiness. While all surveyed organizations offer some form of AI training, only 32% of providers and 30% of payers offer extensive training programs. This lack of preparation is likely a major barrier to scaling AI’s full potential.
