What You Should Know:
– Healthcare delivery organizations (HDOs) are grappling with significant financial, legal, and operational challenges stemming from proposed economic and healthcare policy changes from Congress and the new administration, according to a new KLAS report. This high level of uncertainty, intensified by unrecovered pre-COVID margins, staffing shortages, and rising costs, is forcing HDOs to proactively adapt their strategies.
– The report, “Navigating the Uncertainty of Federal Policy 2025,” based on a survey of 169 HDO decision-makers (including health systems, hospitals, and physician practices), indicates that policy shifts are no longer theoretical; they are driving hard choices.
Planning Through The Fog
HDOs are primarily “planning through the fog” (69%), taking steps despite a lack of clarity on risks. Only a small percentage are “clear and confident” (3%) or “cautious but clear” (7%). Those that are more proactive are predominantly academic or large health systems, focusing on their clinical mission and targeting administrative, IT backlog, and discretionary spending cuts before impacting patient-facing services.
“When a turtle sees danger, they kind of buckle down and get into a shell. In many instances, we are approaching that mindset,” stated a CIO from a payer organization, highlighting the widespread caution.
Policy Shifts Drive Hard Choices and Reconfigurations
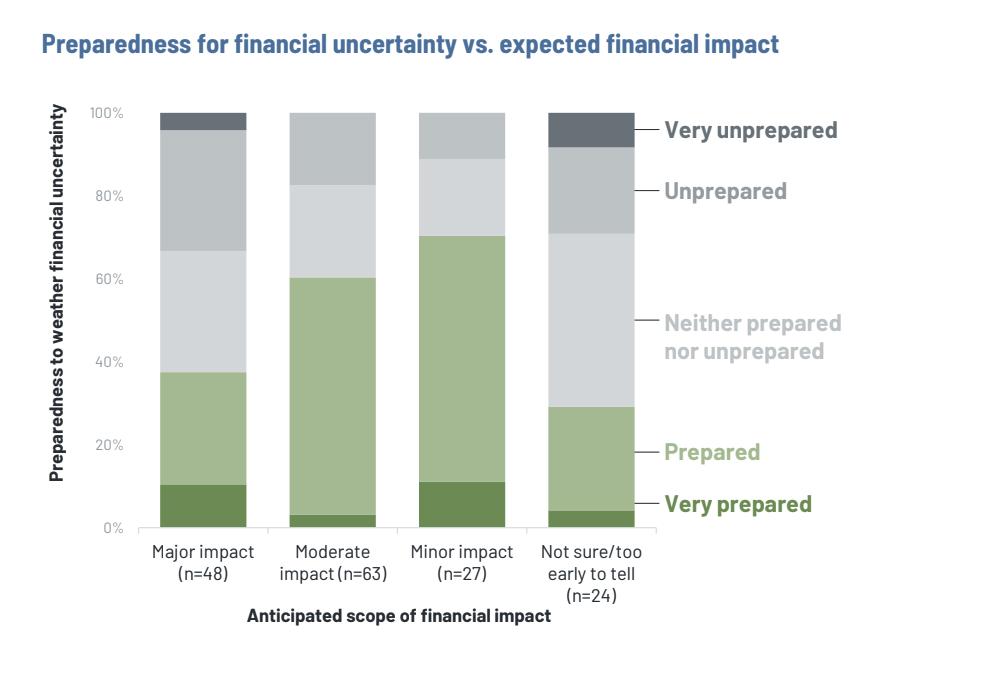
Payment reforms are prompting HDOs to reconfigure services, not just implement cuts. A significant 86% of HDOs have contingency plans in place, often multiple, which include scaling back services, restructuring their workforce, or expanding high-reimbursement lines. This signals a survival strategy with direct implications for patients’ access to care.
The biggest anticipated negative impact from federal policy changes is reimbursement changes (71%). Specifically, cuts to federal Medicaid contributions are a major concern, mentioned 1.5 times more often than Medicare. HDOs express strong emotional reactions, using terms like “devastating,” “catastrophic,” and “crush” to describe potential impacts. Proposed Medicaid eligibility requirements, such as work requirements, could lead to coverage losses and increased uncompensated care for health systems, impacting millions.
Other concerns include 340B reform (19%), reductions in grants/research funding (15%), tariffs/inflation/financial policy effects (13%), and site neutrality (7%). Few HDOs express optimism about proposed government policies, with financial policies and tariffs consistently perceived to have the most negative impact.
Reimbursement Fears Redrawing IT Budgets
Despite uncertainty, 75% of HDOs do not anticipate IT cuts. Instead, they are strategically shifting spending towards vendor partnerships and tools that offer fast, measurable ROI. The focus is on resilience and steady growth over high-risk “big bets”.
The top areas where organizations are increasing IT spend include:
- AI/automation (39%)
- Cybersecurity (31%)
- Increasing hardware/software costs (27%)
Health systems are investing more heavily in AI and hardware/software costs due to tariffs and inflation, while physician practices prioritize cybersecurity and EHR-focused projects.
HDOs Bet Big on AI, Hope for Policy Alignment
The report reveals nearly 40% of HDOs are “betting big” on AI and digital tools to ease administrative loads, often amidst staffing cuts and shake-ups. Investments in infrastructure, cloud, and cybersecurity may be necessary to support these AI initiatives. However, most AI implementations remain in pilot mode, constrained by a lack of funding, standards, or resources for scaling.
AI is most widely adopted by large acute care organizations and larger payers, primarily to improve efficiency, with departmental adoption being the most common strategy. AI is seen as a “bright spot,” with HDOs optimistic that policy changes could loosen AI restrictions.
Value-Based Alignment Evolves into Revenue Strategy
HDOs are rethinking payer partnerships, Medicare Advantage growth, and contract performance, with reimbursement alignment now heavily influencing overall strategic decision-making. Large organizations are closely scrutinizing their payer mix in preparation for potential Medicaid and Medicare reimbursement shake-ups. Some are exploring upside-risk models or capitated arrangements for more revenue stability.
Smaller Providers Face Resource Strain
Even under-resourced smaller provider organizations are engaging in scenario planning, trimming capital spend, or adjusting staffing, but they often lack the extensive resources of larger systems. They are left with limited teams, sparse analytics, and no margin for error, straining their ability to execute strategic plans. These smaller organizations are prioritizing foundational IT infrastructure (88%), clinical quality and safety (72%), and advanced analytics (60%). Their top barrier to digital transformation remains talent shortfalls (41%).
Best Practices to Navigate Financial Uncertainty
The report concludes with key considerations for providers, payers, and vendors navigating this uncertain environment:
- For Providers: Act with clarity and intentionality, even if it means difficult choices. Embrace collaborative partnerships as a lifeline.
- For Payers: Demonstrate transparency and flexibility to strengthen networks. Reimbursement stability should be a strategic conversation, recognizing providers are under pressure.
- For Vendors: Position yourselves as true partners. Tech spend is narrowing but not disappearing, and sales cycles will be driven by strategic clarity and demonstrable cost mitigation. Focus on “growth support” rather than just “efficiency” in messaging.
