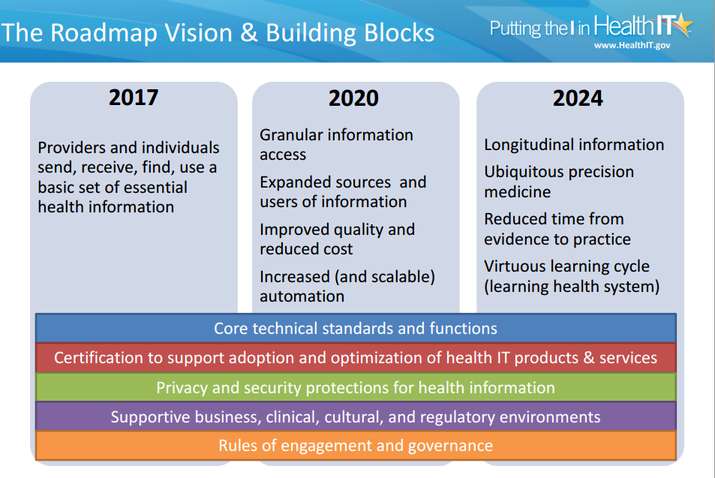
On Wednesday, the Office of the National Coordinator for Health Information Technology (ONC) held the first joint meeting of the Health Information Technology Policy and Standards Committees to discuss future of interoperability in healthcare. During the meeting, the ONC presented some of the early strategic elements of the draft interoperability roadmap proposing key near-term actions and milestones for many of the 3, 6, and 10 year goals. The elements are structured around five critical building blocks for a nationwide interoperable health IT infrastructure:
– Core technical standards and functions
– Certification to support adoption and optimization of health IT products and services
– Privacy and security protections for health information
– Supportive business, clinical, and regulatory environments
– Rules of engagement and governance
“We have heard loudly and clearly that interoperability is a national priority, and that there is value in this effort spearheaded by ONC as the federal government’s coordinator of health IT policy. It is also apparent that there is enthusiasm, capability and a willingness to cooperate and collaborate in ways not previously seen. We are invigorated by the collaborative energy we have seen and experienced over the few months by those who have leaned forward with us,” Karen DeSalvo, ONC National Coordinator stated in a recent ONC blog post.
Draft Health IT Ecosystem Goals
| Stakeholder | 2014-2017 | 2017-2020 | 2020-2024 |
| Individual | Send, receive, find, and use electronic health information |
Electronically contribute to and correct their health information; access shared care plans in standardized electronic format • Increased access to longitudinal health information |
• Regularly track and share electronic information from wearable, implantable, biometric medical devices • Increased access to longitudinal health information |
| Provider | Send, receive, find and use the common MU data set for all patients • Receive electronic notifications when individuals are admitted to or discharged from inpatient care |
Increased granular access to specific health information when/where needed • Automated tools that effectively use electronic clinical data from multiple sources for quality improvement and decision support across care continuum • Seamless remote monitoring and care for through remote devices |
• Increased access to longitudinal health information • Care tailored precisely to each individual based on information about environment, occupation, human services, genomic data, cutting edge research evidence, etc. |
| Population & Public | Information contained in the common MU data set aggregated across communities for population health and quality measurement • Research community accesses aggregations of EHR data in pilots • Notifications based on relevant information are shared seamlessly |
Clinical and administrative data normalized and aggregated across communities to support broad scale value-based payment models • Research community accesses aggregations of standardized EHR data for ongoing research • Public health and other clinical registries receive and make available broad suite of standardized data for use by authorized individuals |
Research community has access to large aggregations of standardized genomic and device data for research purposes • Public health better contains outbreaks and proactively manages disasters with electronic information from many sources |
The draft roadmap is scheduled to be finalized by January 2015 for public comment with the approved version slated for March 2015.
The early draft material of the interoperability roadmap is available for view/download here
