What You Should Know
- The Launch: Optum is rolling out a dual-sided AI strategy to modernize prior authorization: Digital Auth Complete for providers (powered by Humata Health) and InterQual® Auth Accelerator for payers.
- The Provider Impact: By embedding AI directly into the EHR, the provider-side tool has demonstrated a 96% first-pass approval rate in early deployments, aiming to reclaim the average 13 hours per week staff spend on these tasks.
- The Payer Impact: The payer-side solution focuses on regulatory compliance (specifically CMS 0057), reducing review times by 56% while maintaining a strict “human-in-the-loop” policy that forbids AI from auto-denying coverage.
For health systems, the new offering is Digital Auth Complete. Powered by Humata Health, this tool embeds directly into the Electronic Health Record (EHR). The philosophy here is invisibility. “With Optum, our goal is to make prior authorization virtually invisible to providers and patients,” said Dr. Jeremy Friese, CEO of Humata Health.
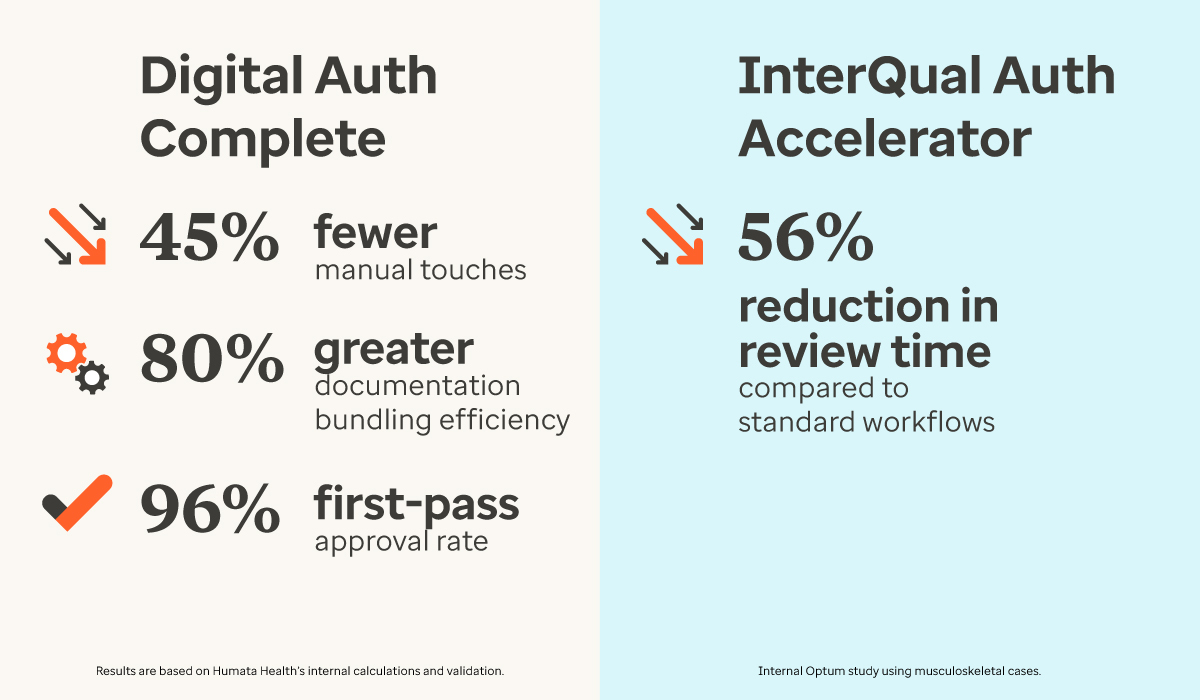
Instead of manual data entry, the AI scrapes the necessary clinical data, applies payer rules, and submits the request automatically. The results from early deployments are head-turning:
- 45% reduction in manual touches.
- 80% increase in processing efficiency.
- 96% first-pass approval rate.
Allina Health, a major Midwest health system, has signed on as one of the first innovation partners to deploy this technology, signaling strong provider-side interest.
For Payers: Speed Without the “Auto-Denial” Risk
For health plans, the pressure isn’t just efficiency; it’s regulatory. The new CMS 0057 requirements mandate that urgent requests be processed within 72 hours and standard requests within seven days.
Optum’s answer is InterQual® Auth Accelerator. This solution uses AI models trained on 50 years of InterQual clinical criteria to convert provider documentation into machine-readable formats. Early results show a 56% reduction in review time, helping payers comfortably meet the new federal speed limits.
Crucially, Optum is addressing the “Black Box AI” controversy head-on. The system is designed with Human-Centered AI principles: it can automate approvals, but it does not auto-deny cases. Any rejection must still pass through human hands, keeping patient care decisions within expert control.
“We’re transforming the prior authorization process to address the friction it causes,” said Dr. John Kontor, SVP of Clinical Technology at Optum Insight.
