What You Should Know:
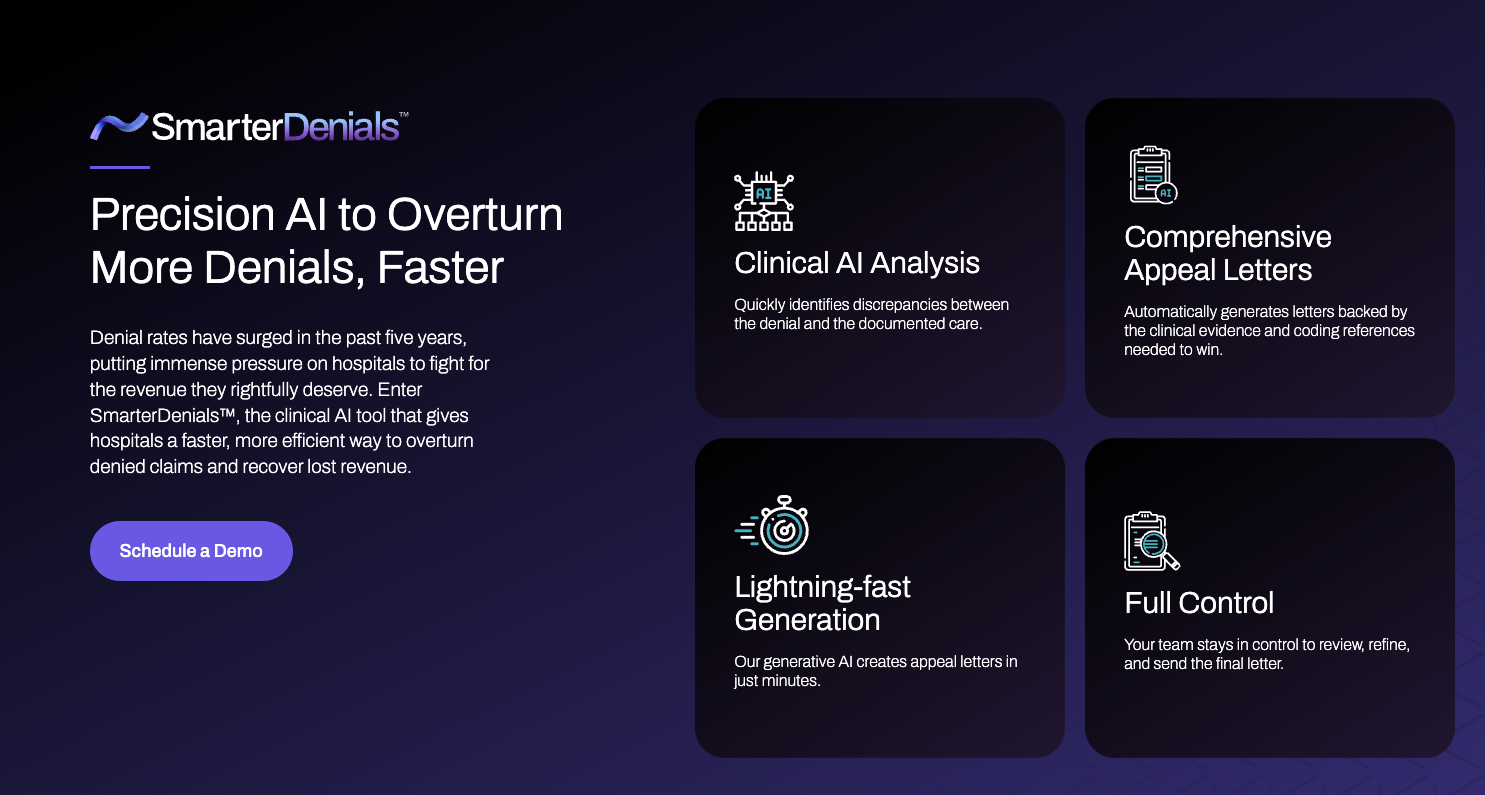
– SmarterDx, a provider of clinical AI for revenue integrity, has announced the launch of SmarterDenials, an innovative AI-driven solution designed to help hospitals fight unjust claim denials.
– With denials on the rise, causing operational disruptions and revenue loss for healthcare providers, SmarterDenials empowers hospitals to generate stronger clinical appeal letters and secure faster and more accurate reimbursements.
Addressing the Growing Challenge of Denials
The healthcare industry is facing a surge in claim denials, with a 20% increase in the past five years. This trend has significant financial implications, costing hospitals over $20 billion annually in efforts to overturn denials. The traditional process of manually reviewing denials and composing appeal letters is time-consuming and inefficient, adding to the administrative burden on healthcare staff.
SmarterDenials: AI-Powered Efficiency for Appeals
SmarterDenials streamlines the appeals process by leveraging AI to:
- Analyze Patient Records: Identify relevant documentation that supports the medical necessity of the denied services.
- Generate Appeal Letters: Create comprehensive and compelling appeal letters in minutes, complete with case-specific clinical evidence and coding references.
- Reduce Administrative Burden: Eliminate the need for manual review and letter composition, freeing up staff time for other critical tasks.
- Accelerate Reimbursement: Increase the efficiency and speed of the appeals process, leading to faster reimbursement for hospitals.
Built on a Proven Platform
SmarterDenials is built on SmarterDx’s proprietary clinical AI platform, which is already used by over 20 leading health systems to improve revenue integrity. This integration ensures seamless access to the solution and leverages SmarterDx’s expertise in healthcare data analytics and AI.
“With SmarterDenials, we’re giving hospitals the tools to fight denials quickly and effectively,” said Michael Gao, CEO and co-founder of SmarterDx. “By helping hospitals better respond to the rising tide of denials and secure the reimbursement they deserve, SmarterDenials helps them focus on what they do best: serving their patients and communities.”
