What You Should Know:
– Value-based care (VBC) has been established as a priority among healthcare organizations and payers as participants have gained more experience in managing their quality metrics and contracts, ultimately realizing returns on their investments.
– For their latest report, KLAS talked to 54 healthcare executives—including CEOs, CFOs, CIOs, CMIOs, COOs, VPs and directors of population health, and VPs of analytics—to gauge how they are moving beyond pay-for-performance into risk-bearing contracts over the next three years and their perceptions on which vendors can help them achieve their upcoming goals with VBC.
Insights Into Provider Burnout and the EHR Experience
Following the COVID-19 pandemic, healthcare organizations have seen massive provider burnout, which ultimately leads to issues with staff shortages and quality of patient care. What can organizations do to alleviate and prevent provider burnout? Since 2018, the Arch Collaborative has conducted research on burnout, with a particular focus on its intersection with the EHR. In the Collaborative’s EHR experience survey, clinicians share their current level of burnout and identify any contributing factors. Using their responses and other measurements from the Arch Collaborative, KLAS’ latest report details what organizations can do to combat provider burnout.
Key findings from the report are listed and explained as follows:
1. Burnout Levelling Out in 2022; Staffing Shortages Rise:
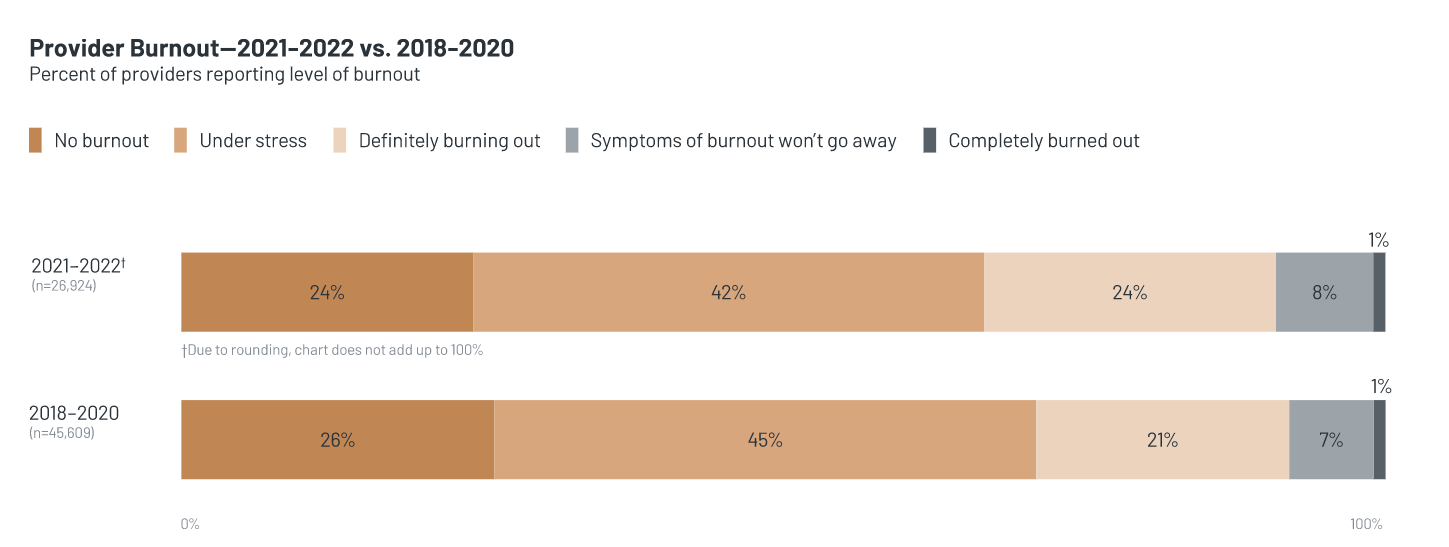
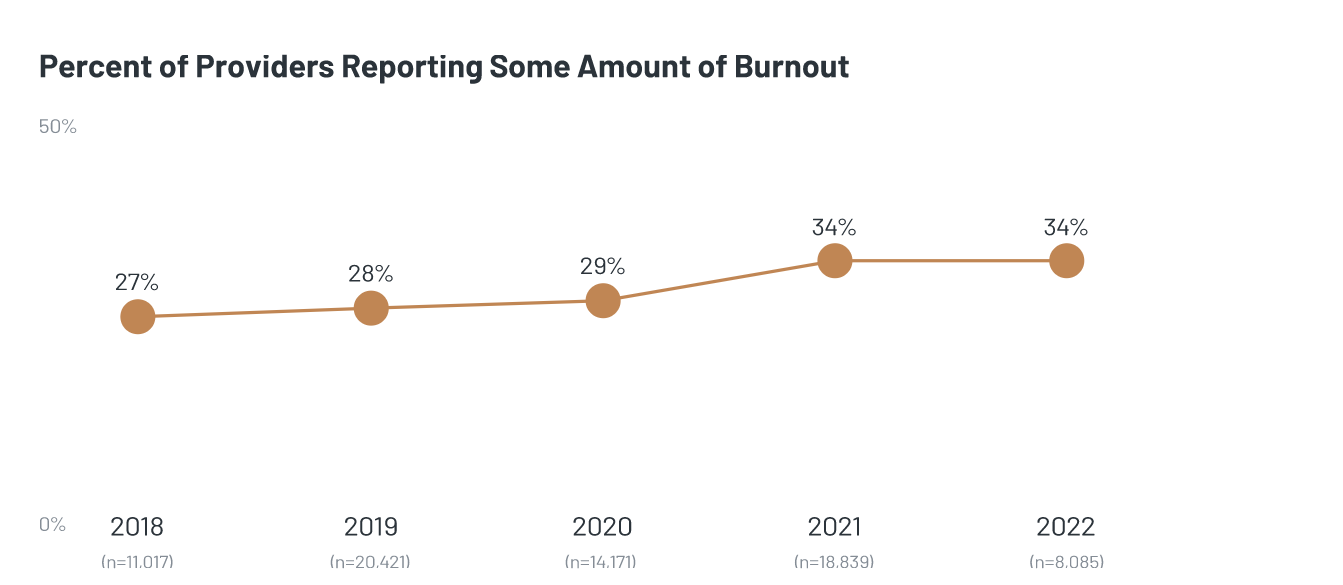
In 2018 when the Arch Collaborative first began measuring burnout, 27% of providers reported at least some degree of burnout (i.e., they chose one of the following responses: definitely burning out, symptoms of burnout won’t go away, or completely burned out). Burnout has since increased, with 2021 seeing a large spike in the number of providers who report at least some amount of burnout. However, rates have leveled off in 2022 and are holding steady at 34%. The same trend is true for other, non-provider clinicians (not measured in this study). It should be noted that since 2020 the percentage of providers reporting higher levels of burnout has increased slightly—particularly those who report they are definitely burning out (up 3 percentage points). Most measured contributors to burnout have become less prevalent than they were at the start of the COVID-19 pandemic. There are a few exceptions. The percentage of providers citing a chaotic work environment as a contributing factor has stayed consistent at 28% pre- and post-pandemic. Staffing shortages—a newly-measured contributor as of 2021—are more frequently reported by all types of clinicians, especially in the last year. In 2022, 40% of surveyed providers said staff shortages contribute to their sense of burnout. As providers report higher degrees of burnout, they are more likely to report a higher number of total burnout contributors.
2. With Foundation of Trust in Leadership/IT, Less After-Hours EHR Time Tied to 19% Lower Burnout:
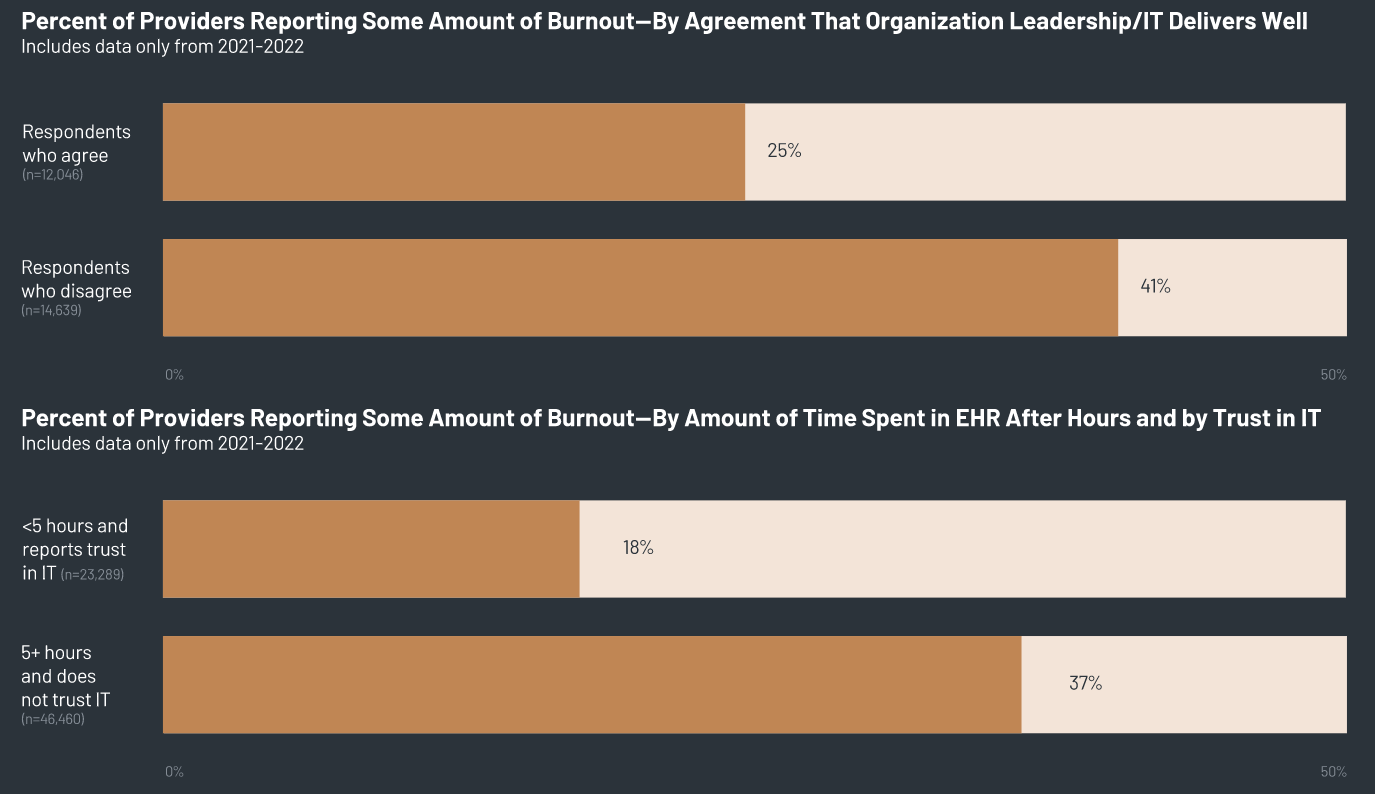
One key to lessening provider burnout is strong provider agreement that their organization delivers well around the EHR—specifically, that the organization has done a great job of implementing, training on, and supporting the EHR. Higher trust in organization leadership/IT in these areas is tied to providers being less likely (by 16 percentage points) to feel burned out. Even among providers who spend more after-hours time in the EHR—who would be expected to have higher rates of burnout— trust in leadership/IT around the EHR is correlated with lower burnout. Providers who chart six or more hours a week but have trust in their leadership/IT experience burnout rates lower than the Collaborative average. Providers who both trust their leadership/IT and chart after-hours for less than five hours per week have an average burnout rate 19 percentage points lower than other providers.
3. Timely and Well Communicated EHR Fixes Strongly Correlated with Lower Provider Burnout:
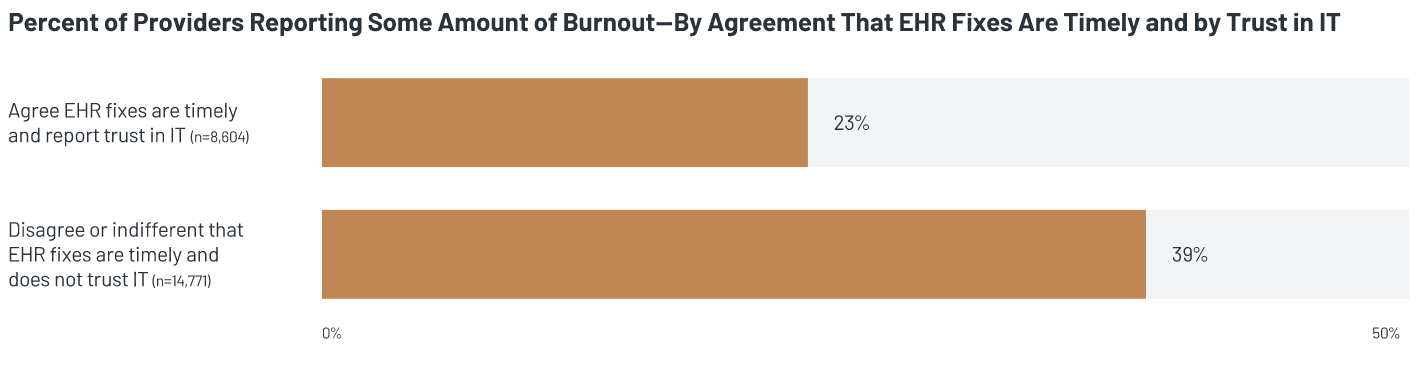
At times, providers can view IT as a black hole, and this dynamic reduces interactions and collaboration between the two groups. However, providers who feel they are supported in their EHR by organizational IT teams report lower levels of burnout. One of the most telling indicators is whether EHR fixes are made in a timely manner. In general, providers who agree with this statement and report trust in IT have an average burnout rate 16 percentage points lower than their peers (see second chart below). Additionally, communication around EHR changes is important; providers who agree changes are well communicated have a burnout rate 11 percentage points lower than those who disagree. When IT and support personnel are more transparent—for example, they update providers regarding requested changes—providers feel more supported and empowered around the EHR experience and their overall experience in the organization. This transparency is also tied to lower burnout.
4. Burnout-Prevention Programs Are Making a Positive Impact:
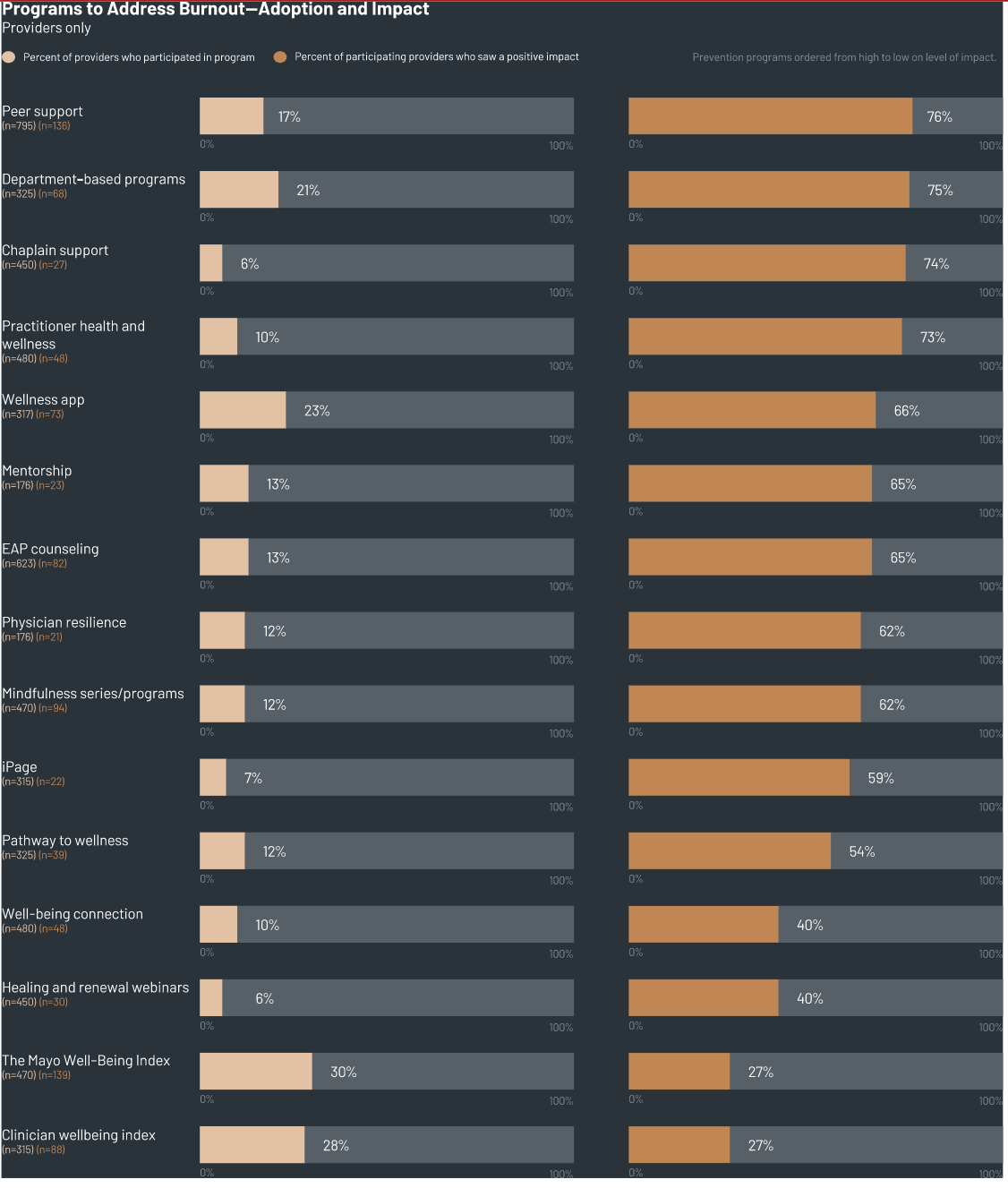
Healthcare organizations have successfully improved their clinicians’ experience at work by implementing programs specific to reducing burnout. Many organizations that participate in the Arch Collaborative have asked their clinicians about participation in a burnout-prevention program and whether the program was helpful. KLAS recommends that all organizations implement one or more of the programs measured in the chart below since all have significant potential to alleviate provider burnout.
The report also included some insights from successful organizations on combating burnout:
1. Ozarks Medical Center (Ozarks) improved provider trust in the organization leadership/IT around the EHR by involving a unified group of providers from across the organization in the decision to switch EHRs. Over 200 clinicians participated in the process. They were separated into 20 different groups to determine which EHR would best suit them. These clinicians were almost unanimous in their decision for a go-forward EHR. Upon implementation of the EHR, Ozarks also required that all clinicians receive a minimum of six hours of EHR training prior to the go-live. Following the change in EHR, provider agreement that the organization delivers well around the EHR improved by 34%, and the overall rate of provider burnout decreased by 10%. Ozarks Medical Center shared that their approach to deciding on the EHR helped unify the organization and strengthened trust in leadership. This in turn made providers more excited about working at the organization and resulted in reduced feelings of burnout.
2. Yuma Regional Medical Center credits their providers’ low burnout rates to the EHR onboarding process and ongoing support—this includes at-the-elbow support from IT technicians and providers’ peers. Yuma has a larger-than-average number of provider leadership positions for an organization of their size (for example, they have 27 staff medical directors), and this means more physicians have the opportunity to lead among their peers. It also results in a more simplified process for providers to reach out to someone when they have questions or concerns about the EHR. This has resulted in reduced feelings of burnout. Traditionally, there is a knowledge gap between IT technicians and providers, so Yuma leverages certified, trained physicians who work with EHR analysts and help design the EHR. This ultimately helps bridge that gap for both sides. One large pain point for Yuma providers was getting patients through care encounters on time because of EHR issues. By implementing a point of contact that providers can speak to after a patient visit, the atmosphere of visits has improved for providers and patients. In the organization’s most recent EHR experience measurement, 19% of their providers reported feeling burned out, which is 14 percentage points lower than the current Arch Collaborative average.
For more information about the report, visit https://klasresearch.com/archcollaborative/report/provider-burnout-and-the-ehr-experience/454
