Hundreds of millions of patients are affected by chronic diseases globally, often suffering from several of them. Despite such a huge opportunity, the coverage of chronic conditions with digital solutions is still below the acceptable level. Today, more than twenty common chronic conditions have its own specificity and are currently at its digital development stage, yet all of them face the same challenges in the digital health market, according to a recent Research2Guidance report.
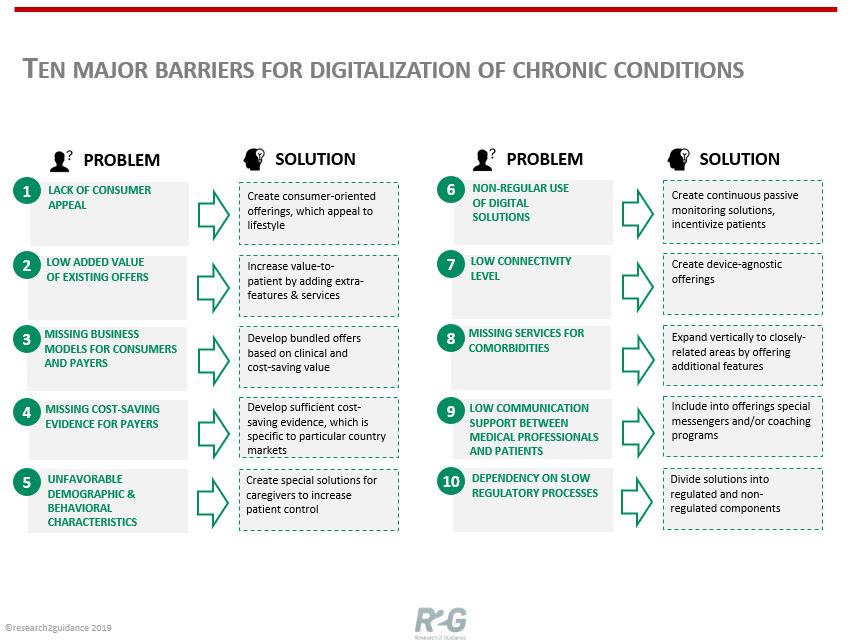
The report, Digital Diabetes Care Market 2018-2022: Ready To Take Off identifies ten major barriers that hinder the development of successful digital ecosystems for the management of chronic diseases:
1. Lack of Consumer Capital
All chronic conditions, apart from digital diabetes, still lack the consumer focus in digital offerings. The main goal of the consumer-oriented approach is to provide and promote a solution that empowers patients to better manage their disease.
2. Low add value
The existing chronic disease apps often create little added value for end users. Most of the currently available solutions offer either basic educational advice or simple tracking based on manual or automated data input.
3. Missing business models for consumers and payers
In the digital health market, payer organizations are now pushing digital services to their member base; however, in the majority of chronic conditions, the reimbursement of digital services is still an issue. Apart from the digital diabetes market, consumer bundle subscription offers or payer models (implemented on the pay-per-member-per-month basis) hardly exist. Digital solution providers should pay more attention to creating reimbursement-oriented packages, which can potentially bundle services, digital content, medical products, and accessories.
4. Insufficient cost-saving evidence for payers
There are many clinical studies across all major chronic conditions that have generated evidence to support efficiency and efficacy of digital solutions in assisting chronic disease patients. What is currently missing is the link to cost savings, which hinders a larger engagement of payer organizations.
5. Unfavorable demographic and behavioral characteristics of patient populations
Patient population characteristics can have significant implications for digitalizing disease management. Solution providers have to find appropriate strategies to increase patient control despite these demographic and behavioral barriers. The development of caregiver solutions is one of the possible responses to this problem. Currently, nearly all of the available solutions are designed for patients or doctors, whereas the role of caregivers in patient management is still underestimated.
6. Non-regular use of digital solutions
Chronic conditions are rather different in terms of usage regularity. In conditions with a limited necessity of regular measurements, the creation of passive monitoring solutions, such as wearable-based measurements, could be one of the means to ensure a constant use of digital solutions.
7. Low connectivity level
Although the use of digital apps in managing chronic conditions is increasing, it is not accompanied by significant growth in the use of connected medical devices, such as blood glucose meters, spirometers, blood pressure meters, etc.
8. Missing services for comorbidities
All chronic conditions have numerous comorbidities, which affect patients no less than diagnosed chronic disease. In many cases, patients suffer from several closely-related chronic conditions at a time. However, solution providers currently focus on primary chronic diseases, offering no services for such conditions as anxiety, depression, obesity, etc. As a result, many chronic condition offerings remain single use case solutions, which do not fully address patients’ needs. Weight-loss, hypertension, and diabetes solution providers are already expanding their primary use cases to other conditions, whereas respiratory conditions still lag behind them
9. Low communication support between medical professionals and patients
Communication between healthcare professionals and patients is seen as the most valuable feature within digital health solutions to drive user engagement and retention. Current digital respiratory solutions offer population management features for HCPs or PDF report generation but do not support direct HCP-patient interaction via chat, email or video call.
10. Dependency on slow regulatory processes
Many digital disease management solutions are treated as medical devices under local regulations, if they include regulated components, such as devices and/or medical products. To avoid extensively long time-to-market, services and/or connected devices can be split into regulated (such as a bolus calculator in diabetes solutions) and a non-regulated (such as behavior change features) components.
Research2Guidance states these barriers is the prerequisite for the success of digital health solutions designed for managing chronic conditions. The market has already seen several successful cases when digital solution providers went beyond the obstacles that were perceived as “natural”.
