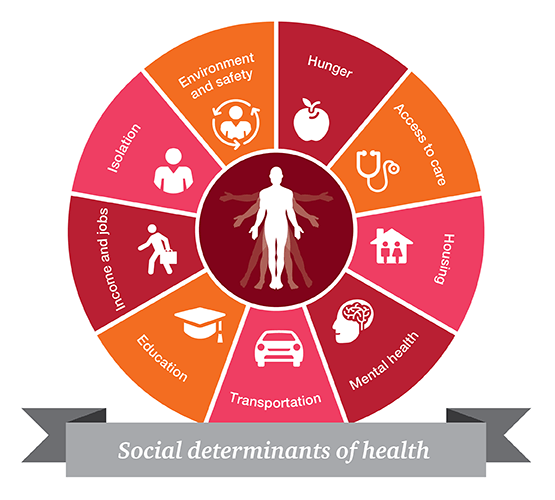
In the value-based care world, cost-effective treatment, quality of care, and patient outcomes determine payment. Social determinants of health (SDOH) represent the economic, psychological, educational, environmental and social barriers that limit healthy behaviors, access to care and adherence to treatment resulting in poor health outcomes. Many stakeholders in health care are trying to address social determinants as part of their value-based care strategy. However, many organizations are challenged with identifying these factors in their populations and do not have the mechanisms to tackle these issues alone.
In the past, social information captured in medical records was limited to drug, alcohol and tobacco use, dietary and exercise habits as well as occupation. Other nonclinical factors such as economic stability, transportation access, food insecurity, or housing security were rarely asked or not documented in a structured way in medical records. Now, with the push to address these issues to improve outcomes, organizations are facing barriers that range from data collection and aggregation to developing solutions that address these problems.
The Challenges of Social Determinants Data Collection
Collecting data on social determinants is difficult due to a lack of consensus on standard assessment tools, little information about best practices for implementing these tools, (DeMilto & Nakashian, 2016) and lack of incentive for providers to spend time collecting this information. If data is collected, it’s happening in silos within health systems, community-based organizations, or government agencies. Aggregating data collected by health systems with that collected by public health, community or consumer organizations is cumbersome due to various systems or manual processes used to collect the data and the lack of standard terminologies used to represent the data.
If a social issue is identified, organizations struggle with what to do next. A provider’s office or hospital system does not have the means to address these issues alone and are not accustomed to working with non-healthcare entities. Collaborative partnerships with social service, community organizations and other business sectors such as housing, transportation, or legal services need to be formed. This requires building relationships, maintaining up-to-date contact information with non-healthcare entities, defining data sharing policies and follow-up from each partner (DeMilto & Nakashian, 2016) (Brennan Ramirez LK, 2008).
To facilitate collaborative partnerships, the state of New York created policies to support the integration of SDOH into the state’s Medicaid system. New York State Department of Health’s Value-Based Payment Medicaid Reform Program mandates that participating organizations address at least one social determinant of health and partner with a community-based organization if engaging in level two or three risk-sharing contracts (New York State Department of Health Medicaid Redesign Team, 2017).
The New York Department of Health Bureau of Social Determinants of Health was created to incorporate community-based organizations into the NY State health delivery system and promote interventions to address SDOH for Medicaid patients (New York State Department of Health, 2018). Managed Care Organizations in the contracts must provide funding to providers or the community-based organization for their SDOH interventions.
An SDOH intervention menu was created and quality measures were identified for organizations to use when implementing these contracts. From policy to practical interventions, New York has created a framework for organizations to be successful when incorporating SDOH into practice.
How to Effectively Scale Data Collection
Current approaches to collecting and using SDOH data have been in point solutions within specific organizations. The major issue is scaling the data collection and distribution for analysis within healthcare settings and action in non-healthcare settings. Reviewing different proposals from various reports, (DeMilto & Nakashian, 2016) (The Commission on Value-Based Care, 2018) (Eckart & Browne, 2018) (Spencer, Freda, McGinnis, & Gottlieb, 2016), a common blueprint for promoting the use of this data includes:
1. Using standardized code systems to represent social determinants. Due to various assessment tools in use, organizations need a mechanism to understand the data.
2. Standardizing data collection. The industry needs to come to a consensus on a standard assessment tool or harmonize questions and answers across assessment tools.
3. Sharing best practices for methods of collection, distribution, and usage of the data.
4. Developing healthcare and non-healthcare (social services, community-based organizations, government agencies) partnerships. These partnerships will need to identify common objectives, define data sharing and privacy policies, and specify the responsibilities of each organization.
5. Developing a public policy to support funding and research for social determinants programs.
6. Developing standard measures to evaluate the effectiveness of programs. There is a lack of standard measures and methodologies today.
Despite the many significant challenges associated with tackling SDOH, it is important that organizations still pursue it as part of their value-based care strategy. Understanding the nonclinical factors that affect patients is critical to encouraging healthy behaviors, improving access to care and increasing adherence to treatment. By following the blueprint outlined above, existing barriers can be slowly broken down and organizations can begin to extensively address these conditions.
About the Author
Lindee Chin, MD is the Senior Clinical Director of Value-Based Care at Edifecs, a health IT company providing a single point solution to connect to all information exchange partners and to ingest, correlate and optimize digital health data. Dr. Chin is trained in internal medicine with expertise in healthcare information technology and quality measurement. Her experience includes the adoption and implementation of electronic health records, development of clinical decision support and quality measurement algorithms, and product development of population health tools.
Works Cited
Brennan Ramirez LK, B. E. (2008). Promoting Health Equity: A Resource to Help Communities Address Social Determinants of Health. Atlanta. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/tools/pdf/sdoh-workbook.pdf
DeMilto, L., & Nakashian, M. (2016). Using Social Determinants of Health Data to Improve Health Care and Health: A Learning Report. Retrieved from Robert Wood Johnson Foundation: https://www.rwjf.org/en/library/research/2016/04/using-social-determinants-of-health-data-to-improve-health-care-.html.
Eckart, P., & Browne, K. (2018, September 4). Unlocking the Value of Data Sharing. Retrieved from dashconnect.org: http://dashconnect.org/2018/09/04/unlocking-the-value-of-data-sharing-series/
Gomez, M. M., Reddy, A. L., Dixon, S. L., Wilson, J. M., & Jacobs, D. E. (2017, March/April). A Cost-Benefit Analysis of a State-Funded Healthy Homes Program for Residents With Asthma: Findings From the New York State Healthy Neighborhoods Program. Journal of Public Health Management and Practice, 23(2), 229-238.
New York State Department of Health. (2018, July). Social Determinants of Health and Community Based Organizations. Retrieved from https://www.health.ny.gov/health_care/medicaid/redesign/sdh/index.htm: https://www.health.ny.gov/health_care/medicaid/redesign/sdh/docs/sdh_bureauslides.pdf
New York State Department of Health Medicaid Redesign Team. (2017, November). DSRIP – Value-Based Payment (VBP) Resource Library. Retrieved from www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/vbp_library/docs/2017-11_final_vbp_roadmap.pdf
Reddy, A. L., Gomez, M. M., & Dixon, S. L. (2017, March/April). The New York State Healthy Neighborhoods Program: Findings from an Evaluation of Large-Scale, Multisite, State-Funded Healthy Homes Program. Journal of Public Health Management and Practice, 23(2), 210-218.
Spencer, A., Freda, B., McGinnis, T., & Gottlieb, M. L. (2016). Measuring Social Determinants of Health among Medicaid Beneficiaries: Early State Lessons. Center for Health Care Strategies, Inc. Retrieved from https://www.chcs.org/resource/measuring-social-determinants-health-among-medicaid-beneficiaries-early-state-lessons/
The Commission on Value-Based Care. (2018). Integrating Health and Human Services: A Blueprint for Partnership and Action. New York: Human Services Council of New York. Retrieved from https://humanservicescouncil.org/reports/
