BCBS AZ’s value-based care program outperformed cohort across cost and quality measures, underscoring program’s effectiveness at improving population health.
Change Healthcare and ACO Partner released the results for the first complete plan year of its novel shared value-based care savings program with Blue Cross Blue Shield of Arizona (BCBS AZ). More than 600 in-network primary care providers treated over 41,500 patients through 2017 leading to the program remitting a total of $1 million to 603 participating providers.
ACO Partner Value-Based Care Organization Background
Established in 2016, ACO Partner is a value-based care organization that is operated by Change Healthcare and Blue Cross Blue Shield of Arizona. ACO Partner is a joint venture of Change Healthcare and Trinnovate Ventures, a subsidiary of BCBSAZ.
ACO Partner contracts independent primary care providers to join the program to earn shared savings and provides them with sophisticated patient data analytics, care coordination, and provider engagement services. Unlike traditional accountable care organizations, providers can earn rewards for value-based performance but are not charged any membership or service fees.
Blue Cross Blue Shield of Arizona Results for Shared Savings Program
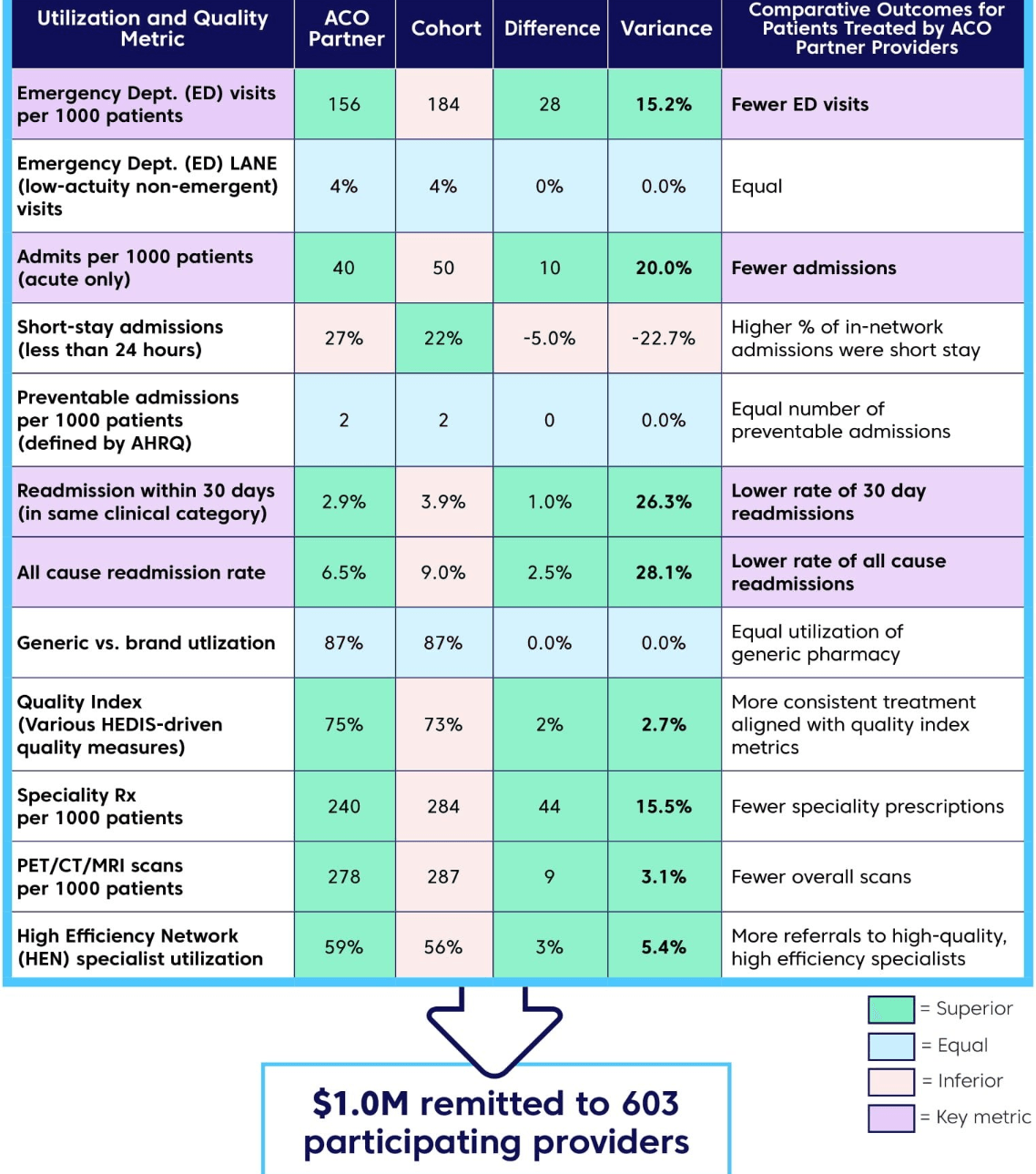
Key results/metrics of the BCBS AZ value-based care program include:
-
Participating providers reported a 26.3% lower 30-day readmission rate and 28.1% lower all-cause readmission rate than their non-participant cohort.
-
The value-based care program reported 20% fewer admissions and 15.2% fewer emergency department visits per thousand treated members.
-
Participating providers also outperformed cohort in the achievement of the program’s Quality Index by 2.7%, and drove lower specialty pharmacy spend, decreased imaging utilization, and more High-Efficiency Network (HEN) specialist referrals.
-
High-performing providers in the program were rewarded for progress toward achieving the “triple aim” of reducing costs, enhancing the patient experience, and improving population health.
-
The providers’ level of performance is reflected across key cost and quality metrics relative to the non-participating cohort. Collectively, these and other cost and quality gains led to the Blue Cross Blue Shield of Arizona Shared Savings Program remitting a total of $1 million to 603 participating providers who treated over 41,500 members.
-
Additionally, the program drove a risk-adjusted claims cost trend from 2016 to 2017 that was 3.7% lower than the cohort trend.
“The model deployed in Arizona, with a focus on care coordination and provider engagement, is achieving the value-based care goals we set when we launched. The program is working for providers and payers, but most importantly for members,” said John Wallace, senior vice president at Change Healthcare and president and chief operating officer of ACO Partner. “The shared savings are just one metric, but when you look at the full range of cost and quality measures tracked through the program, you see that it’s creating more primary care access, and better overall healthcare for members. Leveraging the Change Healthcare portfolio has been a critical element in fostering new levels of payer-provider collaboration and realizing even better efficiency and care quality.”
