Medical patient monitoring devices are poised to disrupt the healthcare industry. According to Markets and Markets, the global market for medical wearable devices is projected to reach $12.1 billion by 2021, with the United States representing the largest market worldwide. With the ability to enhance the healthcare system by aiding in the remote monitoring of patients, wearables provide real-time access to health records and provide quicker diagnosis and treatment of conditions.
They are user-friendly, unobtrusive, and “connected” with features such as wireless data transmission, real-time feedback, and alerting mechanisms. The benefits of utilizing wearable technology extend far beyond the healthcare system, as patients are empowered to take control and monitor their own health.
Despite this promise, most wearables to date have been restricted to the individual wellness and fitness market, and simple adoption of these devices into healthcare is neither a clear-cut nor plausible solution. For wearables in the individual wellness and fitness market, the adoption and transition to a clinical setting requires the passing of rigorous regulatory processes to obtain FDA approval. These regulatory hurdles particularly concern the type and quality of data generated by wearable devices and its relevance and applicability in a clinical setting.
Even if wearables derive medically relevant data, the ability to drive adoption in the healthcare system requires that the information be “billable.” The Centers for Medicare & Medicaid Services (CMS) recently released new payment rules that will give mHealth technology a better shot at reimbursement—an important first step in driving medical wearable implementation in healthcare settings.
Ultimately, medical wearables will be successfully implemented in everyday healthcare when they provide medically relevant data within a structure that pays for more services and makes it easier for providers to both facilitate and bill for them. However, there are a few hurdles that need to be overcome, including:
Problem #1 — Data: The potential of wearables is largely dependent upon the quality of data and its relevance. A wearable will never be billable if it’s not medically relevant. Data derived from current wearables cannot reliably be used to diagnose, treat, or manage health conditions. While the data may be able provide some insight on certain body vitals and metrics, its overall applicability and usefulness to diagnose or treat health conditions is limited. There needs to be demonstrated proof that the utilization of these wearables will be beneficial for patient health.
Although wearables generate copious amounts of data, most is not valuable from a clinical perspective largely because they lack accuracy and consistency in their results. Physicians will not risk the possibility of misdiagnosing or mistreating the patient based on the possibility of utilizing inaccurate and inconsistent data. For wearables to be readily used in healthcare, the first step is to ensure that they provide precise medical grade or clinically relevant data for physicians to effectively utilize in the patient care process.
A second, but equally important, concern comes in the form of security, privacy, and access to data. With a wide range of personal health data available at one’s fingertips, there is a rising concern among users, medical professionals, and the health technology community that this information could end up in the wrong hands.
Patients and physicians alike have pressing questions with regards to who has access to the data, including third parties and who owns the data. Most healthcare systems are not yet equipped with the infrastructure to address these issues on their own.
Wearable technology companies, especially those that want to penetrate the healthcare market, must address these concerns through incorporating security and privacy mechanisms into their solutions. Without implementing security measures, there will be continued reluctance to incorporate wearables into healthcare practices.
Problem #2 — Billing: While the ability to generate accurate, clinically relevant data tackles the first hurdle of integrating wearables into healthcare, the subsequent question then becomes how to incorporate wearables into today’s billing practices. In 2018, CMS will start supporting clinicians who leverage remote patient monitoring tools, such as medical wearables and smart devices at home, and use patient-generated health data in care coordination and management.
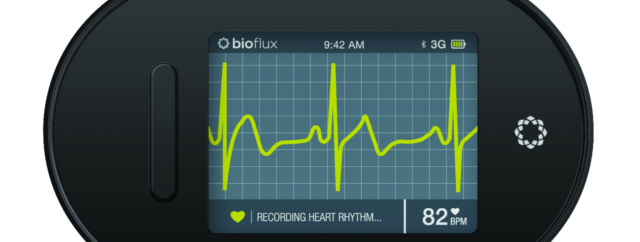
This landmark healthcare development is especially potent for medical wearables, because CMS is positioning remote services, i.e. remote patient monitoring platforms, as distinct from telehealth and telemedicine. CMS is incentivizing the use of more “active devices” that provide real- or near real-time patient generated health data to the clinician or as automated feedback to the patient.
If these devices achieve clinical relevance through benchmarking and FDA approvals, the insurance and healthcare industry will continue to become more inclined to create billing mechanisms that will then open the market for medical-grade wearables.
Today, new remote monitoring solutions are quickly being integrated into existing diagnostic and billing infrastructure of hospitals and physician practices, and are poised to resolve these problems by making it easier to track compliance and health outcomes.
For example, traditional ambulatory arrhythmia monitoring provides inconsistent results and is costly with cardiac-related costs estimated to hit $800 billion by 2030. Also, healthcare providers need to be sure that their wearables meet the requirements as defined within the billing codes.
Every code has specific requirements set out for its use, and what is needed from the device to utilize that code. Validation is achieved when providers meet those requirements and receive FDA approval. CMS has said that it will be finalizing separate 2018 payment for CPT code 99091, which details certain remote patient monitoring.
There is infinite opportunity for medical devices to transform healthcare, but only if they address the concerns around clinical relevance which in turn impacts billability. If wearables become more clinically relevant, there is potential for them to become an instrumental part of our daily lives, ultimately driving down healthcare costs.
If – and when – clinical relevance is achieved, patient compliance will increase because of better patient engagement and understanding of the ramifications surrounding individual choices.
Waqaas Al-Siddiq, Founder and CEO of Biotricity, a developer of professional and personal remote medical monitoring technology engineered to improve people’s lives.
