Connance, a provider of healthcare predictive analytics solutions, has partnered with CareWire, a text-first, mobile patient engagement solution provider, to integrate a new set of predictive analytics into CareWire’s HIPAA-compliant messaging platform for patients. Connance and CareWire are piloting the solution and anticipate general release of the enhanced capabilities in Q4. Connance leverages data science, integrated to workflow to drive enhanced performance. Connance delivers Patient Pay Optimization, Reimbursement Optimization and Value- Based Risk solutions that combine our data, hospital data and consumer data to stratify patients based on social determinants to predict behavior and provide actionable insights to improve net income and patient outcomes.
Integration Details
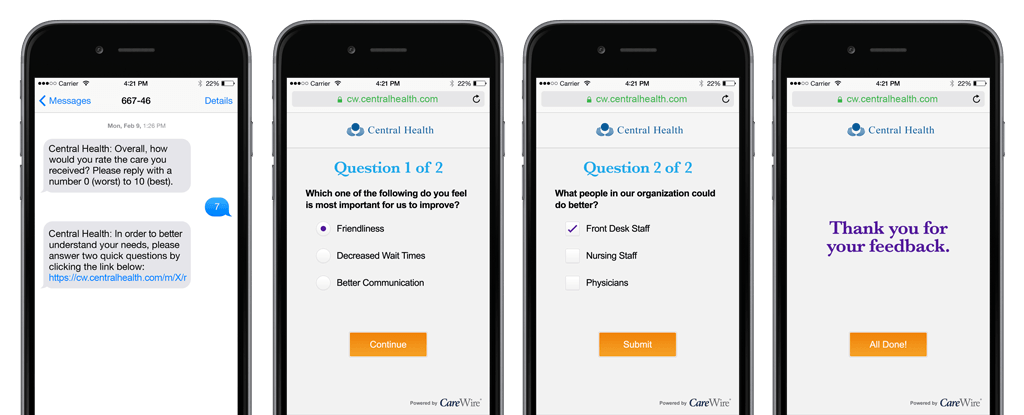
As part of the integration, CareWire will incorporate the Connance predictive analytics solution into its existing platform to further enhance messaging tactics and personalize interactions. Insight into each patient’s socio-demographic and behavioral profile allows CareWire to tailor interactions throughout the continuum of care—including post-surgical/treatment and chronic disease management—to offer the specific programs and interventions that address individual patient needs. For example, if the analytic highlights transportation challenges, the platform will automatically include messages that offer provider sponsored links to transportation alternatives.
Beyond meeting Meaningful Use requirements, value-based care is driving the requirement for healthcare organizations to engage with patients both inside and out of the clinic. Customized text messages personalized to the unique attributes of patients improves impact in meeting compliance and quality objectives and ensuring that important steps in the care plan such as follow up appointments and medication adherence are not missed.
“According to the Centers for Disease Control, socio-demographic and behavioral factors impact up to 70 percent of consumer health,” said Randy Hawkins, Connance chief medical officer. “Access to transportation, financial stability, and food security are factors providers need to understand if we’re going to improve patient outcomes, especially when it comes to managing chronic diseases such as diabetes or congestive heart failure.”
