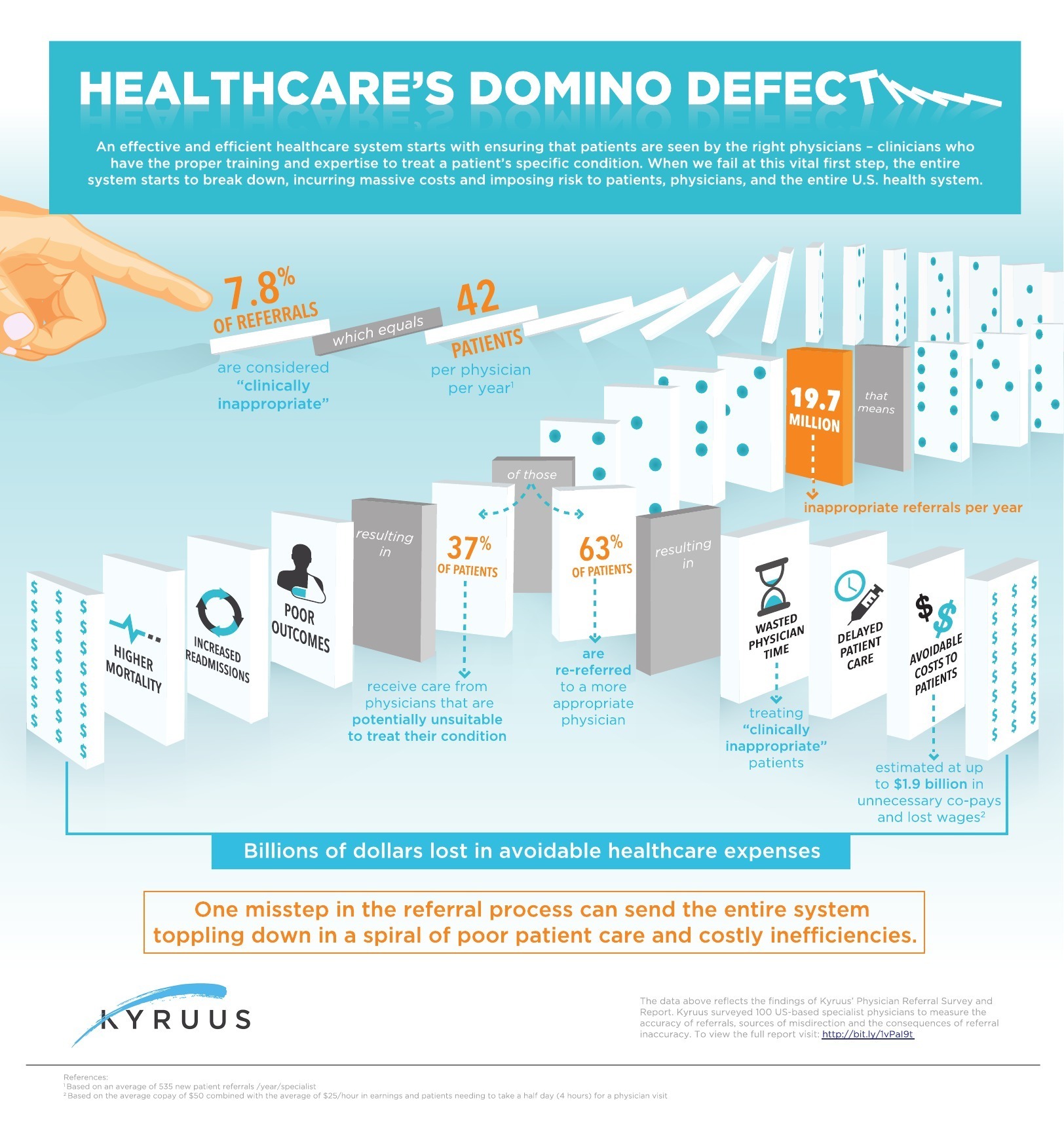
Research from Kyruus highlights how “clinically inappropriate physician referrals” can lead to poor patient care and costly inefficiencies.
Nearly 20 million times a year in the U.S., patients are sent to a doctor who is not the right match for their specific condition. This is one of many key stats in the new physician referrals survey conducted by Kyruus,that highlights the massive issues in the doctor-patient referral system.
Why does this matter? “Clinically inappropriate” referrals can lead to poorer health outcomes for patients, increased hospital readmissions, ineffective use of doctors’ time and unnecessary patient costs, generating billions of dollars in avoidable spending across the entire U.S. healthcare system. The recent Veterans Affairs wait times scandal is an example of the consequences of these inefficiencies. According to ReferralMD, 50% of referrals never result in a doctor’s visit 20% of malpractice claims for diagnosis error involve referral communication deficits.
Key Findings
The Kyruus Physician Referral Survey, which surveyed 100 U.S.-based specialist physicians across 11 medical specialties, found:
Referral Pathways
– 53.8% of referrals received by specialists come directly from other physicians
– Academic medical centers based physicians reported higher rates of referrals via centralized call centers than physicians in private practice, 14.1% vs. 7.8%, respectively
– Subspecialists are more likely to receive their referrals both from referring primary care physicians as well as referring specialists who do not have a further sub-specialty.
Referral Sentiment
– 75 percent of specialists have received at least one “clinically inappropriate” referral in the past year.
– 7.8 percent of all referrals are considered “clinically inappropriate,” which equates to 42 mismatched patients to specialist per year and 19.7 million clinically inappropriate referrals annually nationwide.
– 26.2% of referrals are potentially inappropriate: 18.4% of referrals to specialists in the last year were
considered “somewhat appropriate” while 7.8% are considered “inappropriate”.
– 65% of of clinically inappropriate referrals were either sent to the wrong specialist or subspecialist (48%) or did not require a referral at all (17%).
Outcomes
– When sent a clinically inappropriate referral – 63% of physicians will re-refer the patient to another, more suitable, physician.
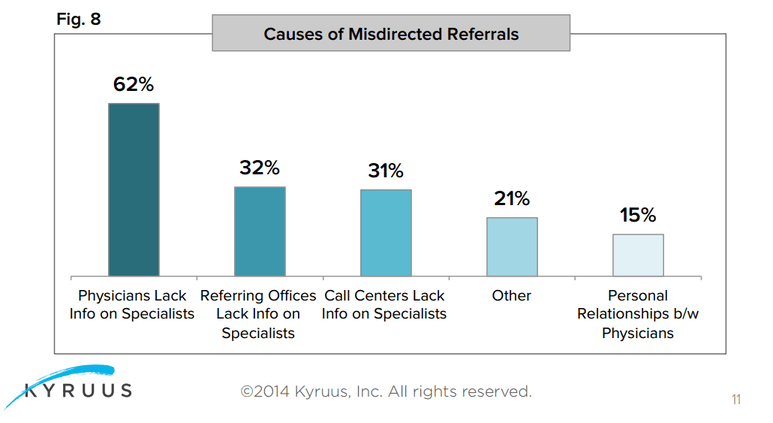
Misdirection Causes
– What causes inappropriate referrals? 87 percent of physicians believe that referral misdirection happens when there is a lack of reliable information about the specialists.
– Insufficient information can be endemic to call centers (31 percent), referring offices (32 percent), or referring physicians themselves (62 percent).
– 15 percent said inappropriate referrals were a result of the referral process relying too heavily on personal relationships between physicians.
– Of the patients who are referred incorrectly, 63 percent are re-referred to more clinically suitable physicians, incurring an estimated $1.9 billion in lost wages and unnecessary co-pays annually.
– The remaining 37 percent who are not re-referred are instead managed by a clinically inappropriate physician, putting quality patient care at risk.
Survey Background/Methodology
In February 2014, Kyruus administered a 15-minute online survey to 100 physicians across 11 medical specialties:
• Cardiology
• Colon & Rectal Surgery
• Dermatology
• Gastroenterology
• Neurology
• Neurosurgery
• Orthopedic Surgery
• Ophthalmology
• Plastic Surgery
• Urology
• Vascular Surgery
The physicians were asked questions about referral methodologies at their institutions or practices, their assessments of the clinical suitability of referrals, and perspectives on the potential causes of referral misdirection.
An infographic illustrating the results of the survey and scope of the problem is shown below:
For a more detailed analysis of the survey findings, the Kyruus Physician Referral Report is available at http://bit.ly/1vPaI9t.
