Throughout the pilot, we encountered several anecdotal examples of how patient engagement apps can impact patients including:
- A man reported that the app helped him understand why he was being admitted so often and why he was on all of his meds.
- A woman took the tablet to lunch with her, using the messaging feature to make sure she didn’t miss her physician during rounds.
- A patient thought he had been misdiagnosed, but was able to look up information about his illness.
- Another spoke about using the tablet to stay connected with his workplace and feel more in control of his life.
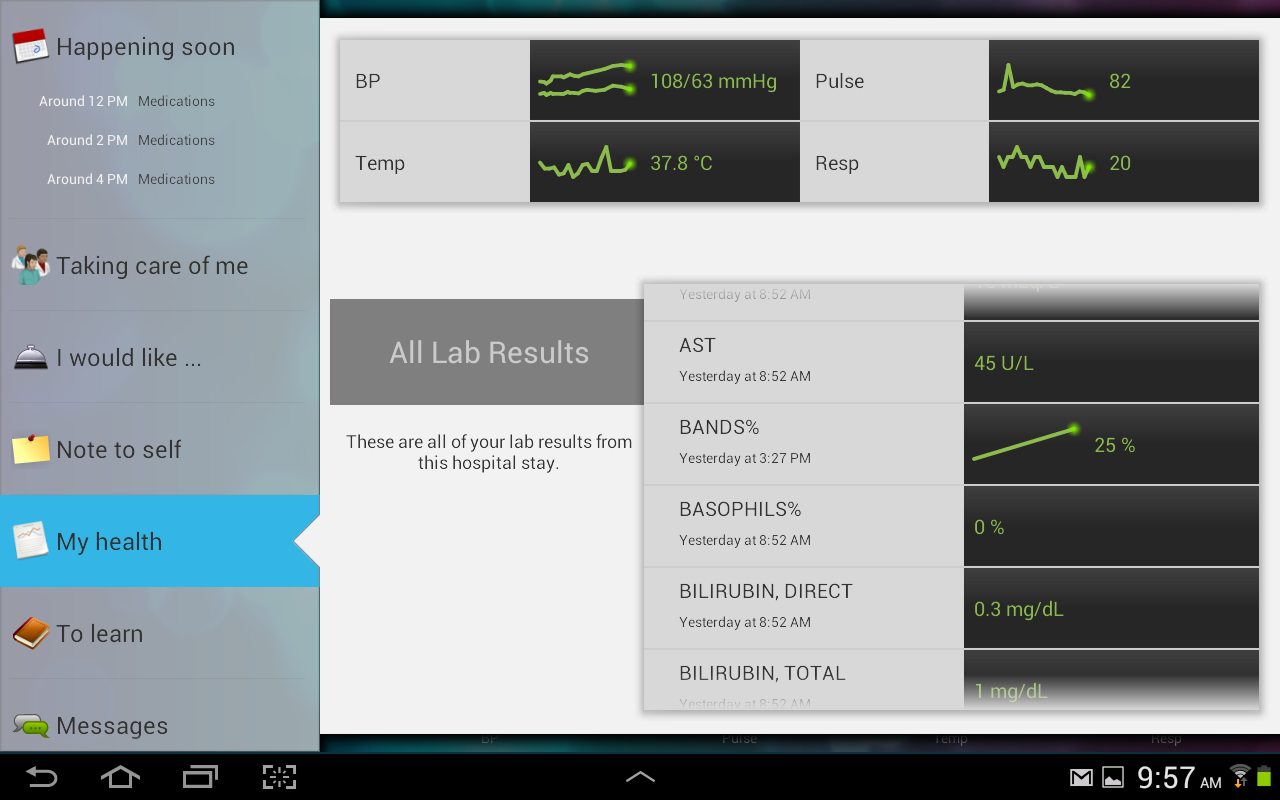
- One patient tracked vital signs and more deeply researched his medications.
- Another liked being able to watch basketball and play games with his son, making his hospital stay less stressful.
The app also seamlessly ties in with patient education offerings we have already employed through our patient portal. Through it, nurses can supply patients with accurate, comprehensive information they need to make smart choices about their health care. Easy-to-understand video educational information provides the tools to educate patients on their condition and help engage them in their own care, leading to improved patient satisfaction and outcomes. Context specific links allow a patient to easily find out more about their medications, labs, and problems.
Patient Engagement beyond the Hospital Stay
Modern healthcare is complex, and many patients struggle to obtain, process, communicate, and understand even basic health information and services. Many also lack health literacy, or a true understanding of their medical conditions. What’s more, the U.S. healthcare system can come up short in addressing patients’ desires and needs, particularly once they leave the hospital. Many practitioners fail to empower patients with educational information they need to make the best post-discharge decisions about their own care and treatment. Even when patients do receive detailed content, they can be overwhelmed or lack confidence in their own choices.
To address this, CHP has linked the MyChart Bedside app to our patient portal. This means that, even after discharge, patients can still access their hospital data using personal devices at home, effectively improving the healthcare experience—even after the stay.
For example, as an Internal Medicine physician, I provide my patients with glucose monitors that offer a 30 to 60 day summary. This lets them collect data at home so I can monitor their progress between visits. If their 30-day average is too high or too low, I know I need to drill down into the data. If it’s average, I know we can continue the current treatment.
Greater Access to Data Equals More Customized Care
Everyone talks about FitBit and other mobile devices that enable patients to monitor and track their health outside the healthcare system. It is even more important to first create a seamless path for clinical data between the four walls of the hospital and the four walls of one’s home to maintain and improve patient outcomes.
High patient satisfaction following the St. Rita’s launch has us optimistic about the system-wide rollout. We are very excited about the potential of this new product to improve patient care. It will continue to help my colleagues and me save time and communicate more effectively with patients. Anything we can do to help patients improve their own care and become more confident about their choices is a win-win. We believe this will improve patient engagement and we’ll get better outcomes because patients will be happier and healthier.
 Stephen Beck, MD, FACP, FHIMSS, currently serves as Chief Medical Information Officer at Catholic Health Partners. He has more than 15 years of experience in planning, implementation, training and follow-up of EHR installations in civilian and military populations and was one of the first physician users of a fully integrated EHR in Southern Ohio. Dr. Beck was among the first physicians to attain CPHIMS certification, has been a content reviewer for the HIMSS National Conference, and chaired the HIMSS National Professional Practice Task Force. He is a Fellow of both HIMSS and the American College of Physicians and serves on the HIMSS Clinical Decision Support Workgroup.
Stephen Beck, MD, FACP, FHIMSS, currently serves as Chief Medical Information Officer at Catholic Health Partners. He has more than 15 years of experience in planning, implementation, training and follow-up of EHR installations in civilian and military populations and was one of the first physician users of a fully integrated EHR in Southern Ohio. Dr. Beck was among the first physicians to attain CPHIMS certification, has been a content reviewer for the HIMSS National Conference, and chaired the HIMSS National Professional Practice Task Force. He is a Fellow of both HIMSS and the American College of Physicians and serves on the HIMSS Clinical Decision Support Workgroup.
[i] “Health Policy Brief: Patient Engagement,” Health Affairs, February 14, 2013.
[ii] Ross, Stephen E., and Lin, Chen-Tan, “The Effects of Promoting Patient Access to Medical Records: A Review,” J Am Med Inform Assoc., 2003 Mar-Apr. 10(2): 129-138.
[iii] http://medcitynews.com/2013/07/reality-check-even-most-wired-hospitals-still-struggle-with-interoperability-patient-engagement/#ixzz2t7w3m4F7
[iv] Carman, Kristin L., Pam Dardess, Maureen Maurer, Shoshanna Sofaer, Karen Adams, Christine Bechtel, and Jennifer Sweeney, “Patient and Family Engagement: A Framework for Understanding the Elements and Developing Interventions and Policies,” Health Affairs 32, no. 2 (2013): 223-31.
