Written by Debbie Gregory
As the mobile health ecosystem grows, it is vitally important to develop these new delivery models with input from a nurse/clinical perspective.
Inside the Hospital
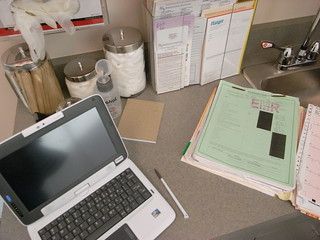 It seems as though the discussions around mobile health are increasing at an exponential rate. The technologies! The access to care! The consumer involvement! The physician tools! There are so many exciting possibilities offered by mobile health in the hospital, but the one corner we need to hear more from is nursing. Most often on the front lines of patient care, nurses are the people using the technologies, facilitating the access, involving the consumer, communicating with physicians, and therefore, it’s imperative that they are directly involved in the creation of mHealth. Excluding nurses from the front-end development and deployment of technologies results in wasted time and money, as technologies can only be successful with the early input from end users.
It seems as though the discussions around mobile health are increasing at an exponential rate. The technologies! The access to care! The consumer involvement! The physician tools! There are so many exciting possibilities offered by mobile health in the hospital, but the one corner we need to hear more from is nursing. Most often on the front lines of patient care, nurses are the people using the technologies, facilitating the access, involving the consumer, communicating with physicians, and therefore, it’s imperative that they are directly involved in the creation of mHealth. Excluding nurses from the front-end development and deployment of technologies results in wasted time and money, as technologies can only be successful with the early input from end users.
An additional complication in the mHealth nursing environment is the disparity of comfort with mobile technology between veteran nurses (who often set pace and provide leadership in a unit) and the new generation of nurses raised on mobile technology (who are full of enthusiasm and eager to embrace technology). These generations can find themselves at odds, and a more intentional inclusion of nursing perspectives – both veteran and new – will help ease this conflict.
There are many methods for increasing nurse involvement in the direction of mHealth, including:
- Hospitals with an Office of Excellence, Office of Lean Process Improvement, Office of Transformation, Office of Innovation or similarly oriented executive function should involve that group in the earliest of discussions regarding new technology. These newly emerging offices are aware of the value in the nursing perspective and understand how to involve nurses to obtain their input on emerging technologies and other workflow innovations.
- An interdisciplinary IT strategic team that includes biomedical, IT, nursing and facility management will give technology initiatives more credibility and protect the integrity of the design intent. Collaboration is the new model, and departments are discouraged from working in isolation to solve problems.
- Include vendors in activities like vendor fairs and educational events. Treat vendors more like co-caregivers and help them to see themselves as co-caregivers when developing apps and devices. Encourage vendors under contract to establish mock rooms in the hospital, so that nurses can experience technologies in a familiar setting, which can aid in their discovery process, uncover valuable feedback for the vendor and improve the usability of the technology.
- Create a Nurse Technology Liaison position – a nurse who is a designated, full-time go-between for clinical staff and IT. For the implementation of any new technology, this position would have an intimate knowledge of clinical workflow and be able to a) advise IT on various aspects and b) help champion the technology and educate nurses once it’s in deployment.
Outside the Hospital
 Another nursing response to the growth in the mHealth ecosystem is the rise of the nurse practitioner (NP). Mobile health is growing outside the hospital as much as it’s growing inside the hospital, and NPs are in a prime position to take on greater primary care roles as care expands outside the hospital.
Another nursing response to the growth in the mHealth ecosystem is the rise of the nurse practitioner (NP). Mobile health is growing outside the hospital as much as it’s growing inside the hospital, and NPs are in a prime position to take on greater primary care roles as care expands outside the hospital.
Take rural care, for example. A shrinking base of family doctors and general practitioners has left people who live outside large cities with diminished medical care and access to health services. Without easy access, rural populations tend to forego medical care. Outfitted with mobile technology, NPs are especially well suited to serve this population. It’s well accepted that NPs can perform about 80% of the work of primary care physicians, including, in many states, prescribing medications. Mobile technology can give nurses access to on-the-go imaging devices, drug formularies, electronic medical records, diagnostic equipment – everything required to provide primary and family care.
Now that technology can guarantee remote connectedness to databases, records, even live specialty physicians, the possibilities for rural care through a “smart health vehicle” and a nurse practitioner are exceptionally exciting. A mobile clinic can deliver healthcare where brick-and-mortar hospitals can’t. Forward-thinking hospitals can get ahead of the game in this area, creating fleets of mobile health vehicles piloted by nurse practitioners, extending a hospital’s reach to 100 miles or more outside of its base city.
The Center for Design Research at the School of Architecture, Design & Planning at the University of Kansas (KU) is currently constructing a prototype of a “smart healthcare vehicle” to accomplish the scenarios described above. Working in cooperation with a national nursing organization, a medical research facility, the medical device industry and several private companies, Kansas University is exploring the convergence of healthcare, communication and transportation technologies to solve healthcare challenges.
Developing a Strategic Technology Master Plan
Predicting what the healthcare delivery system looks like in the future is the question on everyone’s mind. Looking at other major industries, such as banking, gives us a glimpse into the possible evolution of the healthcare industry. Developing a proactive technology strategic master plan that is fluid and flexible will be beneficial for maximizing technology investments and future proofing. Bringing the right people to the table for collaborative discussions and visioning will ensure a consistent and interdisciplinary focus. Key stakeholder groups to include on a technology steering committee are: Facilities Planning and Development, Biomedical Engineering, Clinical Engineering, IT, Nursing, Operational Owners, Supply Chain, Infection Control and Office of Excellence. A complete assessment of current and future technologies should be completed with specific regards to internal resource assessment, financial assessment, and risk assessment. Developing corporate standards and best practices that will drive the process will contribute to the success and return on investments.
Consider an integrative technology approach with the operational intent driving the technology and NOT the technology driving the operations. Technology applied to an efficient process will magnify the efficiency. The same is true for an inefficient process. Clinical efficiencies and process improvement are at the foundation of improved patient care delivery. Technology should be a tool aligned with workflow and operations. Interdisciplinary collaboration to create cohesive solutions will support an integrated sustainable technology ecosystem.

Conclusion
The delivery of healthcare is in a constant state of change in today’s healthcare delivery environment. The one facet that is consistent is the nurse. That is why there will always a huge demand for accelerated nursing programs and training. As mHealth grows and becomes more of a standard practice, it is vitally important to develop these new delivery models with input from a clinical perspective. Every phase of technology development from device development to integration to deployment should have a clinical voice to operationalize the concept related to functionality, best practices, and patient safety. Setting standards for best practices in these emerging practice care models will protect the caregiver as well as the patients and improve care delivery for now and the future.
About Debbie Gregory
 Debbie Gregory is a registered nurse and interior designer. Debbie is co-founder and president of the Nursing Institute for Healthcare Design and is currently senior clinical consultant for Smith Seckman Reid engineering design and facility consulting firm. She has 26 years of experience in nursing as a clinician, healthcare consultant and entrepreneur.
Debbie Gregory is a registered nurse and interior designer. Debbie is co-founder and president of the Nursing Institute for Healthcare Design and is currently senior clinical consultant for Smith Seckman Reid engineering design and facility consulting firm. She has 26 years of experience in nursing as a clinician, healthcare consultant and entrepreneur.
As a nurse and interior designer with a healthcare focus, she provides education for clinical leaders, designers, architects and construction professionals. She serves as a liaison between the clinical community and the design and construction community to improve efficiency and effectiveness through healthcare design.
photo credit: Tricia Wang 王圣捷 via photopin cc
photo credit: juhansonin via photopin cc
photo credit: samsungtomorrow via photopin cc
