What You Should Know:
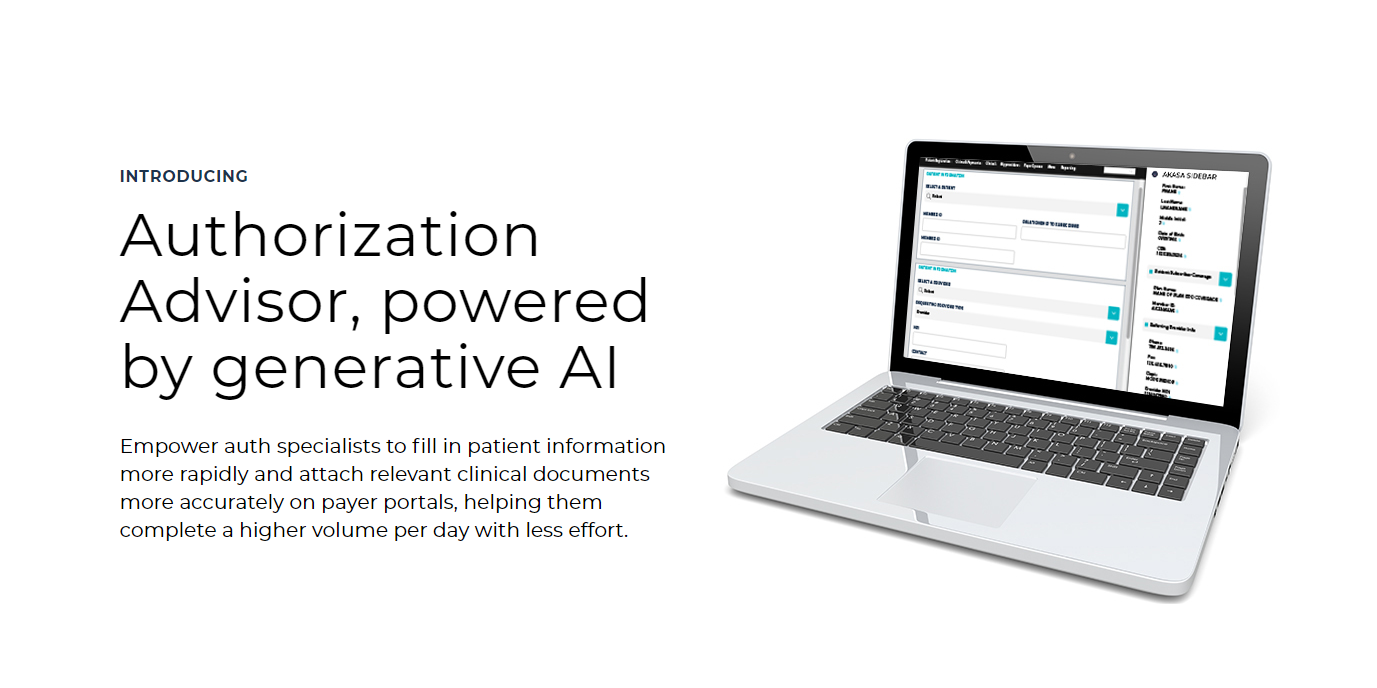
- AKASA, a leader in generative AI (GenAI) solutions for the revenue cycle, today announced the launch of Authorization Advisor™.
- Authorization Advisor tackles the time-consuming and error-prone process of prior authorization, a major pain point for healthcare providers.
Prior Authorization Made Easy with AI
Prior authorization, a process requiring approval from insurers before delivering certain services, is a significant burden for healthcare providers. It
Read More
Revenue Cycle Management | News, Analysis, Insights - HIT Consultant
Feds Launches Investigation of Change Healthcare Cybersecurity Attack
What You Should Know:
- The Department of Health and Human Services' Office for Civil Rights (OCR) has announced an investigation into the recent cyberattack on Change Healthcare, a subsidiary of UnitedHealth Group (UHG).
- The cybersecurity attack has significantly disrupted healthcare billing and information systems nationwide, potentially impacting patient care.
Investigation Focuses on HIPAA Compliance
The OCR enforces the Health Insurance Portability and Accountability Act
Read More
Availity Processes More Than $5B in Claims Stuck with Change Healthcare
What You Should Know:
- The Change Healthcare cybersecurity breach continues to disrupt the healthcare industry three weeks after the initial incident. Hospitals, physicians, pharmacists, and health plans are struggling to maintain operations amidst logistical and financial challenges. Patients nationwide face uncertainty regarding their ability to receive necessary care.
- Availity, the nation's largest real-time health information network, has emerged as a key resource in helping these
Read More
HIMSS24: CodaMetrix Secures $40M for AI-Driven Medical Coding Solutions
What You Should Know:
- CodaMetrix, a provider of artificial intelligence (AI) solutions for healthcare revenue cycle management, has announced the successful closing of its $40 million Series B funding round led by Transformation Capital with participation from existing investors SignalFire, Series A lead, and Frist Cressey Ventures.
- The Series B funding round will fuel further development of CodaMetrix's AI-powered platform, designed to streamline medical coding, improve data quality,
Read More
Frazier Healthcare Acquires RevSpring to Bolster Payment Solutions in Healthcare
What You Should Know:
- Frazier Healthcare Partners, a leading healthcare investment firm, announced today the successful acquisition of RevSpring.
- RevSpring, a provider of end-to-end communication and payment solutions for healthcare and financial services companies, will join Frazier's portfolio.
Frazier's Investment Fuels RevSpring's Future
The acquisition brings together RevSpring's established presence in the communication and payment solutions market with Frazier's deep
Read More
R1 RCM Forms Special Committee to Evaluate $5.8B PE Firm Buy-Out Offer
What You Should Know:
- R1 RCM Inc. (NASDAQ: RCM), a provider of healthcare revenue cycle management solutions, announced the formation of a special committee comprised solely of independent directors.
- The new committee will evaluate strategic options for the company in response to a recent $5.8B buy-out offer from private equity firm New Mountain Capital.
Responding to New Mountain Capital
On February 26, 2024, New Mountain Capital filed a Schedule 13D/A with the Securities and
Read More
Change Healthcare Attack: UHG Announces Restoration Timeline & Provider Relief
What You Should Know:
- UnitedHealth Group (UHG) announced today significant progress in restoring Change Healthcare systems following a cyberattack that disrupted healthcare claims and payment processes nationwide.
- UHG urges all payers to adopt similar funding programs to address the critical short-term cash flow needs of healthcare providers.
Restoration Timeline
Pharmacy Services: Electronic prescribing, claim submission, and payment transmission are fully operational as of
Read More
DeepScribe and AWS Partner to Advance AI-Powered Medical Documentation
What You Should Know:
- DeepScribe, a pioneer in AI-powered medical documentation, today announced a collaboration with Amazon Web Services (AWS) aimed at accelerating the secure scaling of large language models (LLMs) within the healthcare sector.
- The strategic partnership will integrate AWS HealthScribe into DeepScribe's platform, fueling the development of even more advanced AI-assisted clinical documentation solutions.
Scale Generative AI in Healthcare
DeepScribe utilizes a
Read More
CPSI Rebrands as TruBridge, Unifying Solutions for a Streamlined Future in Healthcare
What You Should Know:
- CPSI (NASDAQ: CPSI) announced a strategic rebranding, transitioning to TruBridge, Inc. ("TruBridge") effective March 4, 2024.
- The rebrand reflects a commitment to streamlining its offerings, strengthening its market presence, and driving future growth by creating a unified identity.
A Unified Vision for Healthcare Solutions
The new name, TruBridge, reflects the company's commitment to building a bridge between efficient financial management and quality
Read More
Maverick AI and ImagineSoftware Partner to Automate Medical Coding with Gen AI
What You Should Know:
- Maverick Medical AI ("Maverick"), a provider of an autonomous AI-powered medical coding platform, today announced a strategic partnership with ImagineSoftware, a provider of revenue cycle management (RCM) technology in the United States.
- The strategic partnership aims to automate the coding process, maximize revenue recovery, and optimize workflows for healthcare providers nationwide.
The Challenge: Manual Coding in a Digital Age
The healthcare industry
Read More