What You Should Know
- The News: A new report by KLAS Research validates the performance of Suki, an AI clinical intelligence platform, across three major health systems: FMOL Health, McLeod Health, and Rush University System for Health.
- The Numbers: The systems reported significant ROI, including a 26.8% reduction in documentation time and monthly revenue gains exceeding $1,000 per provider due to improved coding and volume.
- The Takeaway: Ambient AI has graduated from “experimental pilot” to “operational necessity,” proving it can simultaneously alleviate physician burnout and improve financial viability.
For the last three years, the healthcare technology sector has been awash in promises regarding Generative AI. The pitch is seductive: an invisible digital scribe that listens to patient exams, writes the notes, and frees doctors from their keyboards. But for hospital executives and technology leaders, the question has shifted from “Can it do it?” to “Does it actually pay for itself?”
A new validation report released by KLAS Research offers a definitive “Yes.”
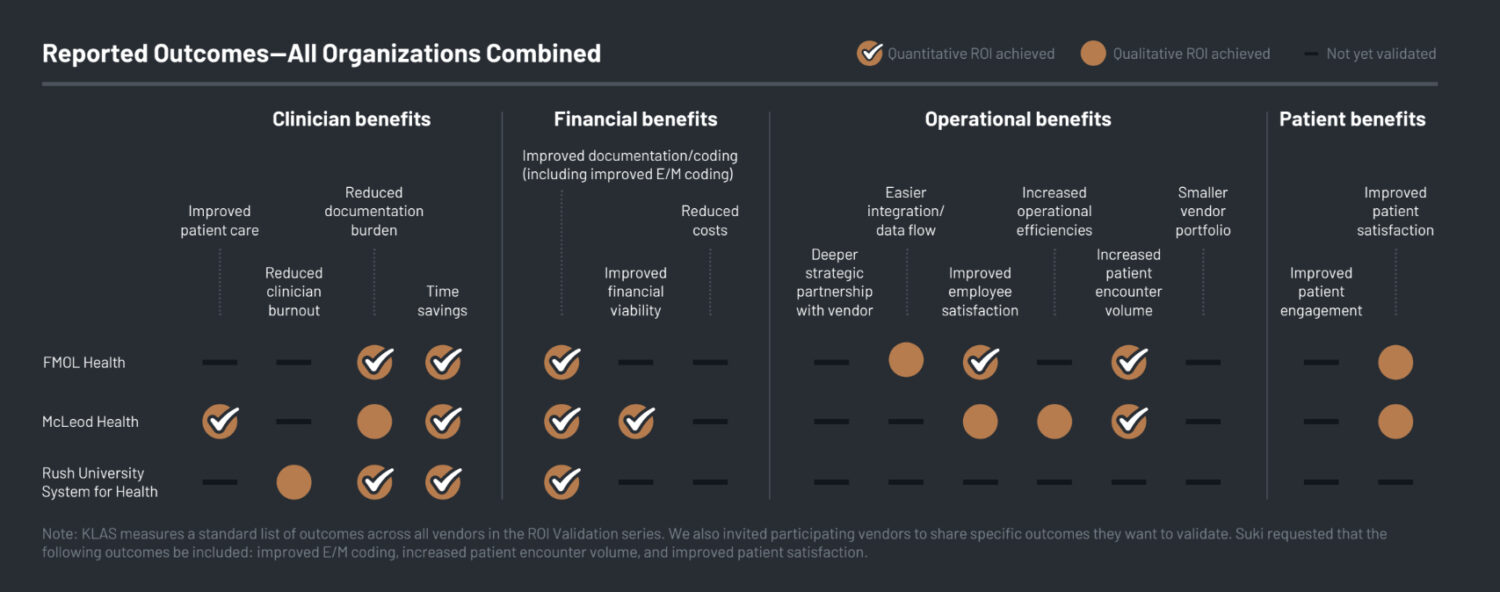
Analyzing data from three large health systems—FMOL Health, McLeod Health, and Rush University System for Health—the report moves beyond anecdotal praise to hard metrics. The findings suggest that Suki, an AI-powered clinical intelligence platform, is delivering on the dual mandate of modern health tech: reducing the cognitive load on clinicians while driving measurable revenue recovery.
The Financials: Coding Accuracy Drives Revenue
The most compelling data in the KLAS report concerns the bottom line. Historically, digital scribes were viewed as a cost center—a perk to keep doctors happy. The data from McLeod Health and FMOL Health flips this narrative, framing the technology as a revenue driver.
McLeod Health recorded a net gain of $1,004 per provider per month. This wasn’t magic; it was math. By using Suki, the system saw a shift in Evaluation and Management (E/M) coding. For established patients, Level 3 codes dropped by 18.2%, while Level 4 and Level 5 codes increased by 7.3% and 5.0% respectively. This indicates that the AI is capturing the true complexity of patient visits that harried human doctors often under-document.
FMOL Health saw a similar trajectory, reporting an $862 monthly revenue increase per user. The AI’s ability to capture detailed clinical nuance allowed for a 6.5% increase in established Level 4 patient visits.
The Efficiency Dividend: Time Given Back
While CFOs look at the revenue, CIOs and CMOs are looking at the “Time Tax” of electronic health records (EHRs). The report highlights that ambient AI is successfully successfully eroding this tax.
- McLeod Health: Achieved a 26.8% reduction in time spent on notes, saving providers roughly 3.6 hours per month. Perhaps more importantly, 89% of their providers now spend less than five minutes per note.
- FMOL Health: Reported a 21% reduction in time spent in notes and a massive 43% decrease in notes left open for more than seven days.
- Rush University System for Health: saw a 5.5% increase in same-day chart closure, a critical metric for billing cycles and care continuity.
The qualitative impact of these statistics is profound. At FMOL Health, 100% of surveyed users reported improved work-life balance. In an industry plaguing by burnout, a tool that eliminates “pajama time”—charting at night after dinner—is a retention asset.
Operational Impact: The Volume Lever
One of the fears regarding AI efficiency is that systems will simply force doctors to run faster on the hamster wheel. However, the data suggests that when the documentation burden lifts, capacity expands organically.
At McLeod Health, there was an 18.3% increase in patient encounters per month. FMOL Health saw a 22% organic increase in patient volume. Crucially, FMOL leadership noted this increase occurred “without added pressure from the organization”. When clinicians aren’t drowning in paperwork, they naturally have the capacity to see more patients, improving access to care.
The Last Mile: Patient Experience
The report also addresses the “screen barrier”—the phenomenon where doctors spend more time looking at the computer than the patient.
McLeod Health measured a Net Promoter Score (NPS) of 65 from patients whose doctors used the AI. For context, an NPS above 50 is considered excellent. Patients and providers alike reported better eye contact and more engaging conversations because the technology receded into the background.
Ambient AI Market Maturation
The KLAS report on Suki signals a maturation point for the market. We are no longer discussing if ambient AI works, but how it scales. The participating health systems have moved from pilots to broader rollouts—McLeod expanding to 249 users and Rush to over 240.
As healthcare systems face tightening margins in 2026, technologies that cannot prove their ROI will face the chopping block. This data suggests that ambient AI is safe from the cut.
C-Suite Lessons: Best Practices for AI Adoption
For a Chief Medical Officer or CFO, the lessons from these systems are clear:
- Don’t Chase Pure Price: Success came from choosing a responsive partner that iteratively refined note structures based on clinician feedback.
- Longitudinal Metrics Matter: Use at least three months of data to account for onboarding variability; focusing only on initial time savings will miss the larger coding and revenue story.
- Coalition of the Willing: Start with motivated volunteer clinicians to set strong adoption patterns before attempting an enterprise-wide mandate.
