What You Should Know:
– A new market survey from Carta Healthcare reveals that hospital leaders are overwhelmingly rejecting fully autonomous AI in favor of “hybrid intelligence” models that pair technology with clinical expertise.
– With 62.5% of respondents citing data misinterpretation as a critical risk of “black box” systems, the industry is cementing a preference for AI that augments rather than replaces human decision-making.
The End of the “Black Box”: Why Hospitals Are Rejecting Autonomous AI for Hybrid Intelligence
For the better part of a decade, the hype cycle surrounding healthcare technology has promised a future where Artificial Intelligence would automate the hospital, replacing manual workflows and diagnosing patients with algorithmic precision. However, new data released today suggests that the industry is waking up from that dream—and realizing that without a human pilot, the plane shouldn’t fly.
According to the November 2025 AI in Hospitals & Health Systems market survey released by Carta Healthcare, the industry has reached a consensus: “Good AI is not good enough.” Hospital leadership is decisively shifting toward Hybrid Intelligence—a model that integrates AI speed with human judgment—while expressing deep skepticism toward autonomous, “black box” solutions.
The Trust Deficit in Autonomous Systems
The survey, conducted by Reaction Data, paints a stark picture of the limitations of fully automated systems in high-stakes clinical environments. Despite the influx of capital into autonomous AI, only 12.5% of health organizations reported that these tools have delivered the most value in their operations to date.
The hesitation isn’t born of technophobia, but of risk management. The data reveals that 62.5% of healthcare leaders identify “misinterpretation of data” as the top risk when AI operates without human oversight. In a clinical setting, a data hallucination isn’t just a glitch; it is a patient safety liability.
This finding marks a maturity point in the sector. The initial rush to deploy AI is being tempered by the reality of complex clinical data, which often requires contextual understanding that current Large Language Models (LLMs) and algorithms struggle to provide independently.
The Rise of the “Force Multiplier”
The survey data supports a new operational paradigm: AI as a teammate, not a replacement.
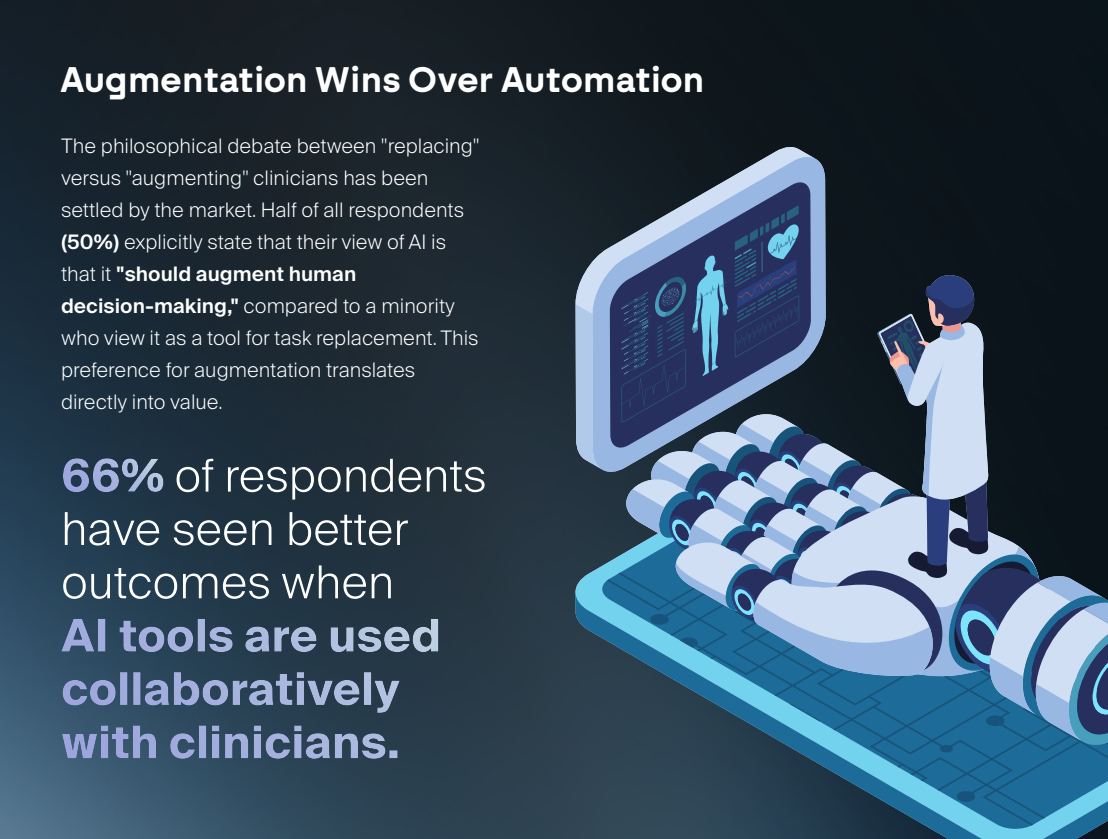
- 75% of respondents view clinician involvement in AI design and deployment as “critically important.”
- 75% rely on human validation to ensure AI outputs are trustworthy.
- 50% explicitly stated that AI’s role is to “augment human decision-making,” rejecting the “task replacement” narrative.
“Healthcare leaders aren’t looking for a magic switch to automate healthcare,” says Brent Dover, CEO of Carta Healthcare. “They want a force multiplier—AI that respects clinical expertise, demands human validation, and integrates seamlessly into existing workflows.”
Dover’s comments align with a broader trend of “Human-in-the-Loop” (HITL) workflows. Hospitals are increasingly looking for solutions that use AI to handle the heavy lifting of data abstraction and processing, while reserving the final mile—validation and decision-making—for expert clinicians.
Why Hybrid Intelligence is the Winning Strategy
The preference for Hybrid Intelligence stems from the unique nature of healthcare data. Unlike financial or retail data, clinical records are often unstructured, messy, and laden with nuance. “Black box” AI, which obscures how it reaches conclusions, is proving insufficient for this environment.
By contrast, the hybrid model creates a safety net. It offers the speed and scale of technology—automating the 80% of routine work—while ensuring that the critical 20% requiring judgment is vetted by a qualified professional.
As the market heads into 2026, the vendors who succeed will likely be those who stop promising full automation and start delivering tools that make clinicians faster, smarter, and safer. As the Carta data shows, the winning strategy isn’t about removing the human; it’s about building a better team.
